S. 2420: No Surprises Act Enforcement Act
The No Surprises Act Enforcement Act (S. 2420) aims to enhance regulations around health care billing practices, with a focus on "balance billing." This occurs when patients receive a surprise medical bill for services provided by out-of-network providers, typically in emergency situations or when a patient unknowingly receives care from a provider not covered by their health plan.
Key Provisions of the Bill:
1. Increased Penalties
The bill proposes to:
- Raise penalties for group health plans and health insurance issuers that fail to comply with balance billing requirements. Specifically, penalties could reach up to $10,000 per violation rather than the previous maximum of $100.
- Extend these increased penalties to nonparticipating providers that fail to adhere to regulations regarding billing.
2. Additional Penalties for Late Payments
If a plan or provider fails to make required payments after an Independent Dispute Resolution (IDR) process determines a payment amount, the bill stipulates:
- The entity must also pay a penalty of three times the unpaid amount.
- Interest will also apply to late payment penalties.
3. Reporting and Transparency Requirements
The legislation mandates transparency in health care billing through:
- Annual reporting to Congress regarding audits of health plans to track compliance with the new provisions.
- A requirement that the Secretary of Health and Human Services submits biannual reports on audits and enforcement actions taken regarding these billing practices.
4. Provisions Related to Air Ambulance Services
For air ambulance services, the bill reinforces similar penalties and payment requirements, ensuring providers comply with payment timelines and reporting requirements.
Relevant Companies
- HCA: As a major healthcare provider, HCA may face increased penalties under this legislation, which could impact their operational costs and billing practices.
- UHS: Universal Health Services, as a hospital management and healthcare service provider, could also be affected by new penalties related to balance billing violations.
- CNC: Centene Corporation, which provides various health insurance products, may need to modify its billing practices to comply with the enhanced regulations under this bill.
This is an AI-generated summary of the bill text. There may be mistakes.
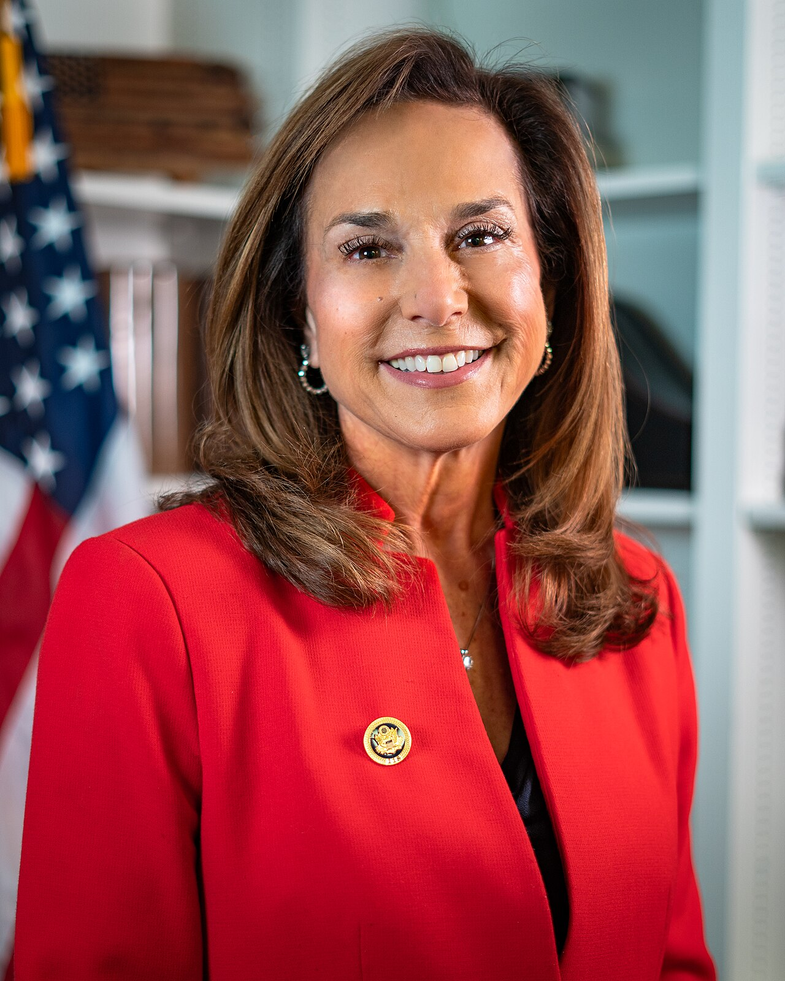
Sponsors
2 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Jul. 23, 2025 | Introduced in Senate |
| Jul. 23, 2025 | Read twice and referred to the Committee on Health, Education, Labor, and Pensions. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.