S. 297: Prostate-Specific Antigen Screening for High-risk Insured Men Act
This legislation, known as the Prostate-Specific Antigen Screening for High-risk Insured Men Act, aims to amend the Public Health Service Act to ensure that group health plans and health insurance providers are required to cover prostate cancer screenings. Here are the main points of the bill:
Objective
The primary goal of the bill is to mandate health insurance coverage for prostate cancer screenings for men deemed at high risk, without requiring any cost-sharing (such as co-pays or deductibles) from these insured individuals.
Target Population
The bill specifically focuses on:
- Men aged 40 and older who are at high risk for developing prostate cancer, including:
- African-American men
- Men with a family history of prostate cancer
Health Findings
The legislation cites several key findings about prostate cancer, including:
- Prostate cancer is the second leading cause of cancer death in men in the U.S.
- More than 310,000 men are expected to be diagnosed with prostate cancer in 2025.
- Survival rates are significantly higher when cancer is detected early.
- Many men do not show symptoms until the disease has advanced.
- African-American men have a higher risk of being diagnosed and dying from prostate cancer compared to White men.
Coverage Requirements
The bill modifies existing health coverage requirements under the Public Health Service Act by:
- Requiring health plans to cover evidence-based preventative care and screenings for prostate cancer specifically for high-risk men.
- Ensuring that no costs are passed on to these individuals for such screenings.
Effective Date
The provisions of this legislation are set to take effect for plan years beginning on or after January 1, 2025.
Other Clarifications
The bill also clarifies that health plans are not restricted to providing only the screenings recommended by the United States Preventive Services Task Force and may provide additional coverage as necessary.
Relevant Companies
- UNH - UnitedHealth Group: As a major health insurance provider, UnitedHealth Group would likely need to adjust their coverage policies to comply with this bill, potentially impacting their cost structure and service offerings.
- CNC - Centene Corporation: Centene, which focuses on managed care and government programs, may need to revise its health insurance plans to include the mandated prostate cancer screenings.
This is an AI-generated summary of the bill text. There may be mistakes.
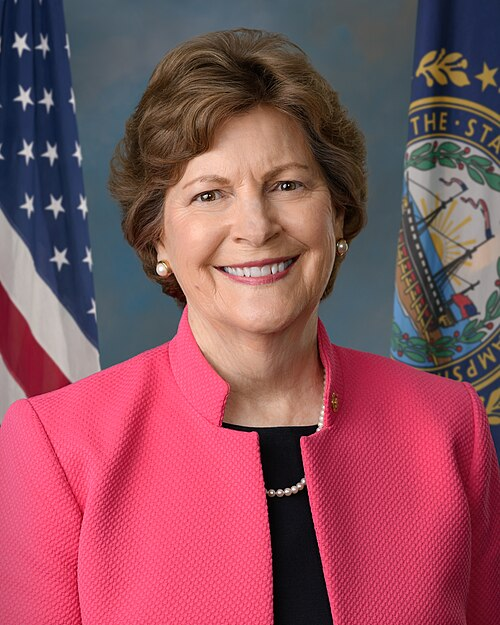
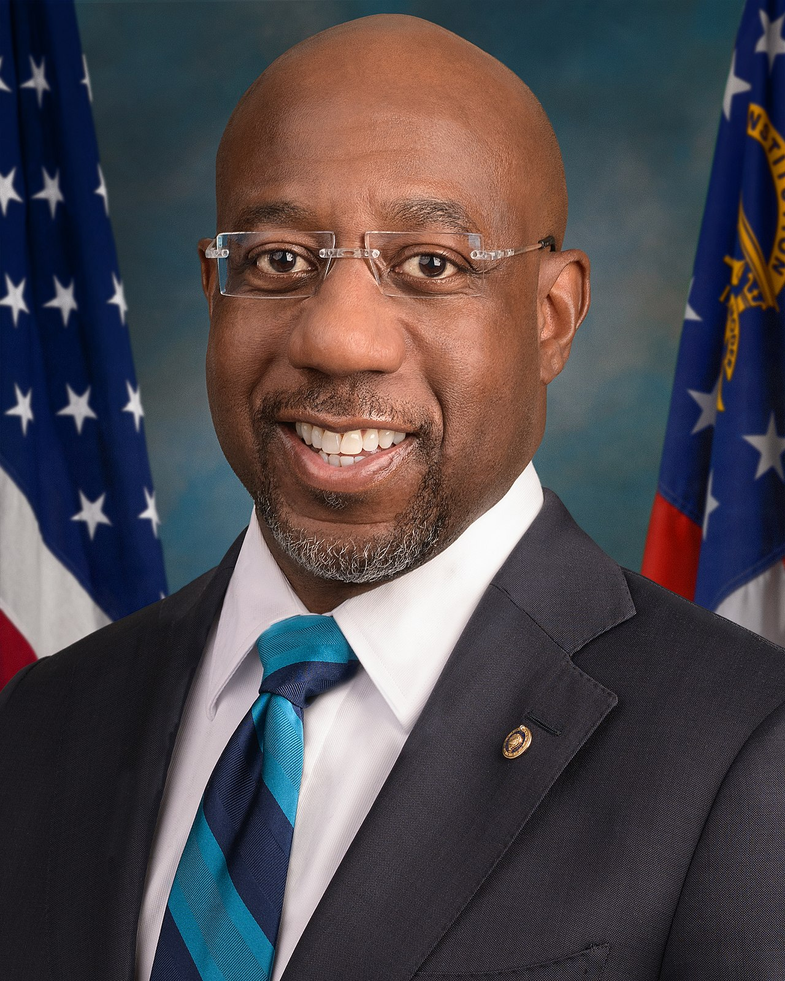
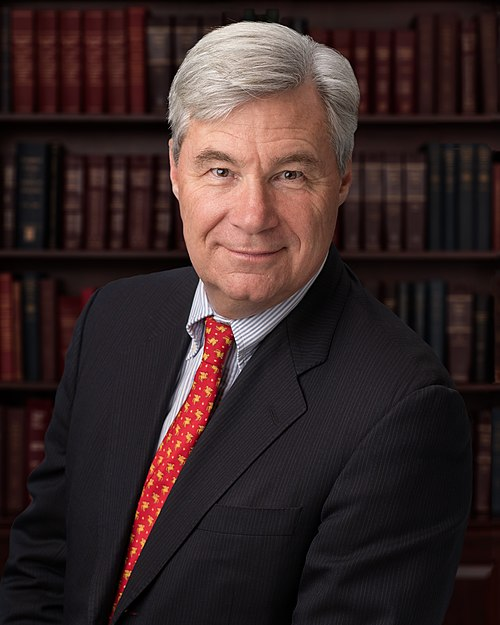
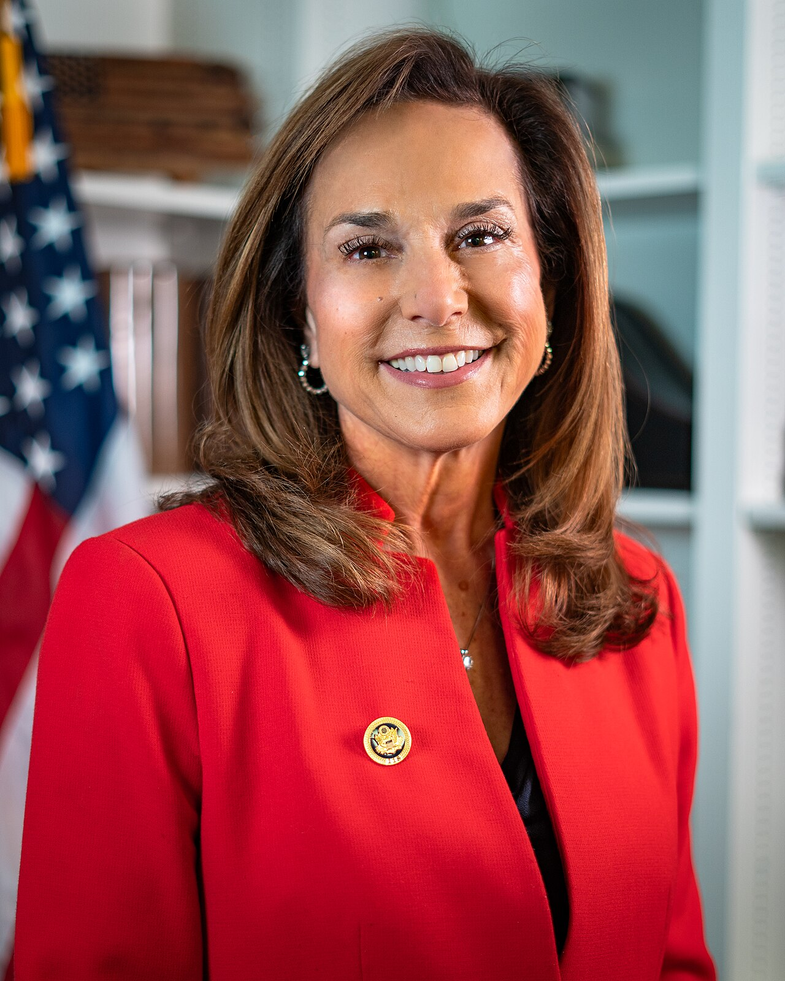
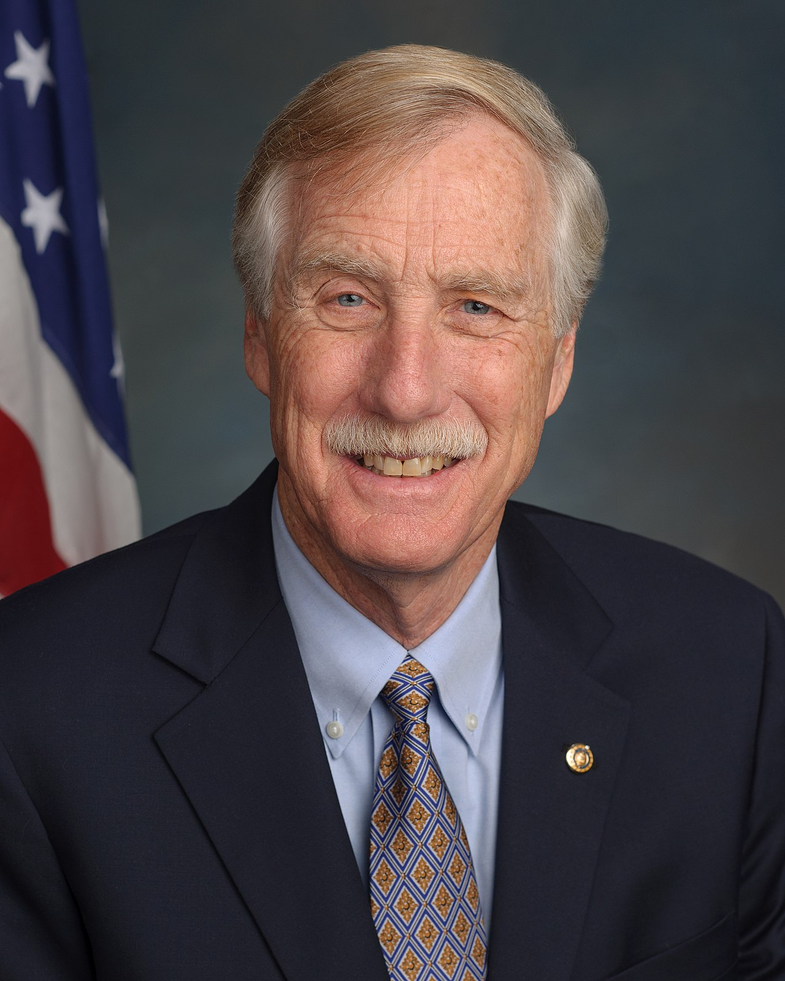
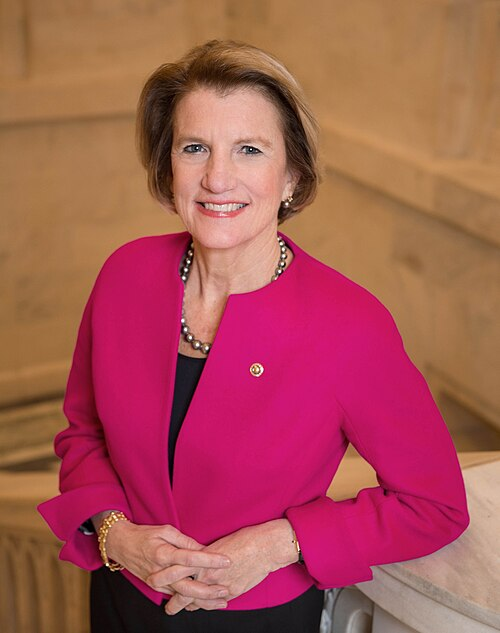
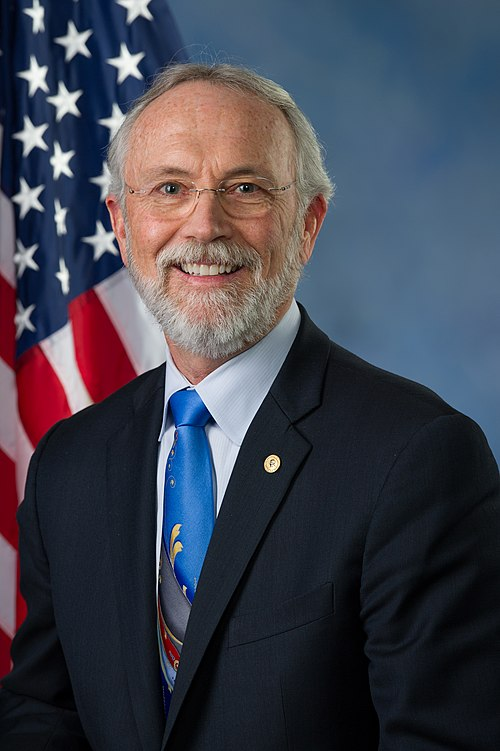
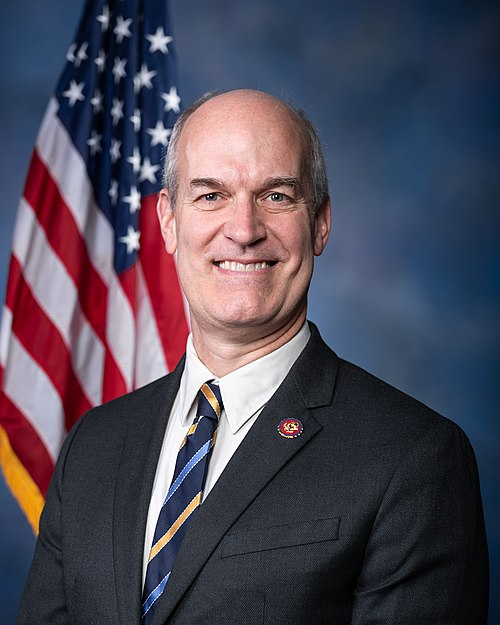
Sponsors
7 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Jan. 29, 2025 | Introduced in Senate |
| Jan. 29, 2025 | Read twice and referred to the Committee on Health, Education, Labor, and Pensions. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.