S. 1105: No Unreasonable Payments, Coding, Or Diagnoses for the Elderly Act
This bill aims to amend the Social Security Act's provisions regarding Medicare Advantage, which is a program that offers health coverage to seniors through private insurers. The proposed changes focus on improving the way payments are determined for health plans by using more accurate diagnostic data and reducing the potential for inflated coding, which can sometimes lead to higher payments than warranted.
Key Provisions of the Bill
Use of Two Years of Diagnostic Data
The bill introduces a requirement that starting in 2026, the Secretary of Health and Human Services must use two years of diagnostic data when adjusting risk payments for Medicare Advantage plans. This means that the payment rates for these plans will be based on a more comprehensive view of patients' health over a longer period, rather than relying on limited or outdated data.
Exclusion of Certain Diagnoses
Another significant change is the proposal to exclude diagnoses that are obtained from chart reviews and health risk assessments when determining payment adjustments for Medicare Advantage plans. Again, this rule would come into effect in 2026. This aims to ensure that only diagnoses that are established through actual patient interaction, rather than administrative reviews, are considered in the payment models.
Application of Coding Adjustments
Additionally, the bill mandates that the Secretary assess the differences in coding practices between Medicare Advantage plans and traditional Medicare providers. This assessment would inform adjustments to ensure that coding disparities do not unfairly influence risk scores and payments. The results of this evaluation would be publicly reported, thus providing transparency about how coding practices may affect payments to different health plans.
Goals of the Bill
The overall intent of the bill is to promote more equitable and accurate payment models within Medicare Advantage, reduce potential abuses related to coding, and ultimately improve healthcare delivery for the elderly by ensuring that funding reflects the actual health status of enrollees.
Implementation Timeline
Most provisions outlined in the bill are set to take effect starting in 2026. This gives stakeholders time to adapt to the changes and ensures a smoother transition to the new system.
Relevant Companies
- AET (Aetna Inc.) - As a major player in the Medicare Advantage market, changes to payment methodologies could affect their revenue and strategies in how they manage care for patients.
- CNC (Centene Corporation) - Centene, which provides Medicare Advantage plans, might see impacts in their billing and reimbursement processes under new risk adjustment criteria.
- UNH (UnitedHealth Group Incorporated) - UnitedHealth, one of the largest health insurers, may need to adjust their coding practices and strategies based on the new evaluation requirements set forth in the bill.
This is an AI-generated summary of the bill text. There may be mistakes.
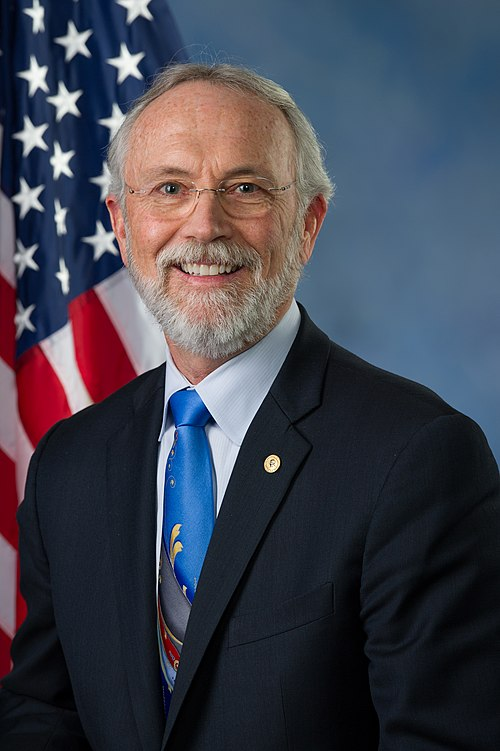
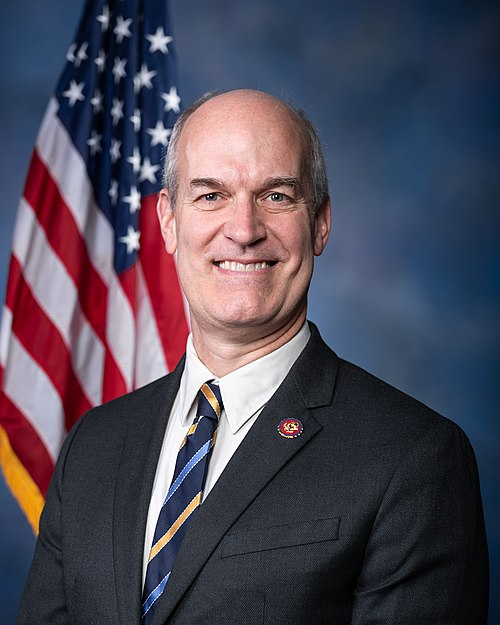
Sponsors
2 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Mar. 25, 2025 | Introduced in Senate |
| Mar. 25, 2025 | Read twice and referred to the Committee on Finance. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.