H.R. 6010: To amend the Internal Revenue Code of 1986 to extend and modify the enhanced premium tax credit, and for other purposes.
This bill aims to amend the Internal Revenue Code of 1986 to make significant changes to health care policies, specifically focusing on premium tax credits and Medicare Advantage risk adjustments, as well as fraud prevention in health plan enrollments. Here are the key points:
1. Premium Tax Credit Modifications
The bill introduces temporary premium percentages for the years 2026 and 2027. The premium tax credits, which help reduce the cost of health insurance, will see the following changes:
- Household incomes up to 150% of the poverty line will have a premium percentage of 0%.
- For incomes between 150% and 200% of the poverty line, the premium percentage will initially be 0% and then rise to 2%.
- For incomes between 200% and 250%, premiums will initially be 2% and rise to 4%.
- Those with incomes from 250% to 300% will see an increase from 4% to 6%.
- For incomes between 300% to 400%, the percentage will start at 6% and go to 8.5%.
- Finally, for incomes from 400% to 600%, the premium percentage will be capped at 8.5%.
These adjustments are intended to apply starting tax years after December 31, 2025.
2. Changes to Medicare Advantage Risk Adjustment
In order to improve the risk adjustment framework for Medicare Advantage plans, the following amendments are proposed:
- Using two years of diagnostic data for risk adjustment calculations starting in 2026.
- Excluding diagnoses gathered from chart reviews and health risk assessments in determining payment adjustments, which is designed to streamline risk assessment further.
- Introducing a coding adjustment that considers discrepancies in coding patterns between Medicare Advantage and traditional Medicare to ensure that payment accurately reflects the risk of enrollees.
3. Reducing Fraudulent Enrollment in Health Plans
This section focuses on minimizing fraudulent practices by enhancing regulations for agents and brokers involved in health plan enrollments:
- Introducing civil penalties ranging from $10,000 to $50,000 for agents or brokers who provide incorrect information due to negligence.
- For knowingly providing false information, higher penalties may apply, including fines up to $200,000.
- Establishing criminal penalties for agents and brokers engaged in willful fraudulent actions during health plan enrollments, which may include imprisonment for up to 10 years.
Additionally, there are provisions to enhance consumer protections during the enrollment process, requiring more rigorous verification of enrollments and ensuring that changes to coverage maintain transparency and consumer consent.
4. Consumer Protections and Transparency
The bill requires the establishment of a verification process for agent-assisted enrollments and mandates that agents and brokers provide better documentation during the enrollment process. This includes:
- Ensuring that individuals are notified promptly about enrollment changes.
- Requiring agents to provide evidence of consent from individuals they assist in enrolling.
- Creating a registry of agents, brokers, and related organizations to maintain accountability and transparency.
- Implementing audit processes to monitor agent compliance and identify potential fraud.
Relevant Companies
- UNH: UnitedHealth Group might be impacted as their revenue could be affected by changes in Medicare Advantage risk adjustments and premium tax credits.
- ANTM: Anthem, Inc. could see shifts in enrollment patterns based on new enrollment processes and penalties, which might alter how brokers operate.
- CNC: Centene Corporation could be affected by changes in Medicare Advantage risk adjustment methodologies affecting their plan offerings and profitability.
This is an AI-generated summary of the bill text. There may be mistakes.
Sponsors
12 bill sponsors
-
TrackSam Liccardo

Sponsor
-
TrackDon Bacon

Co-Sponsor
-
TrackVicente Gonzalez
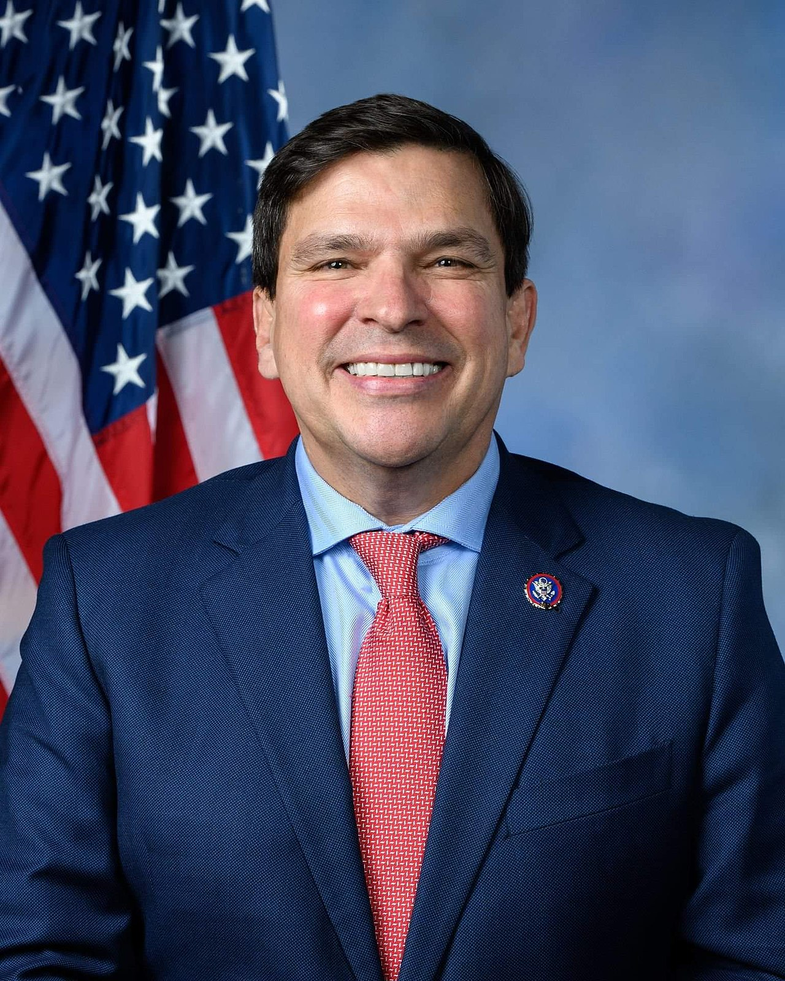
Co-Sponsor
-
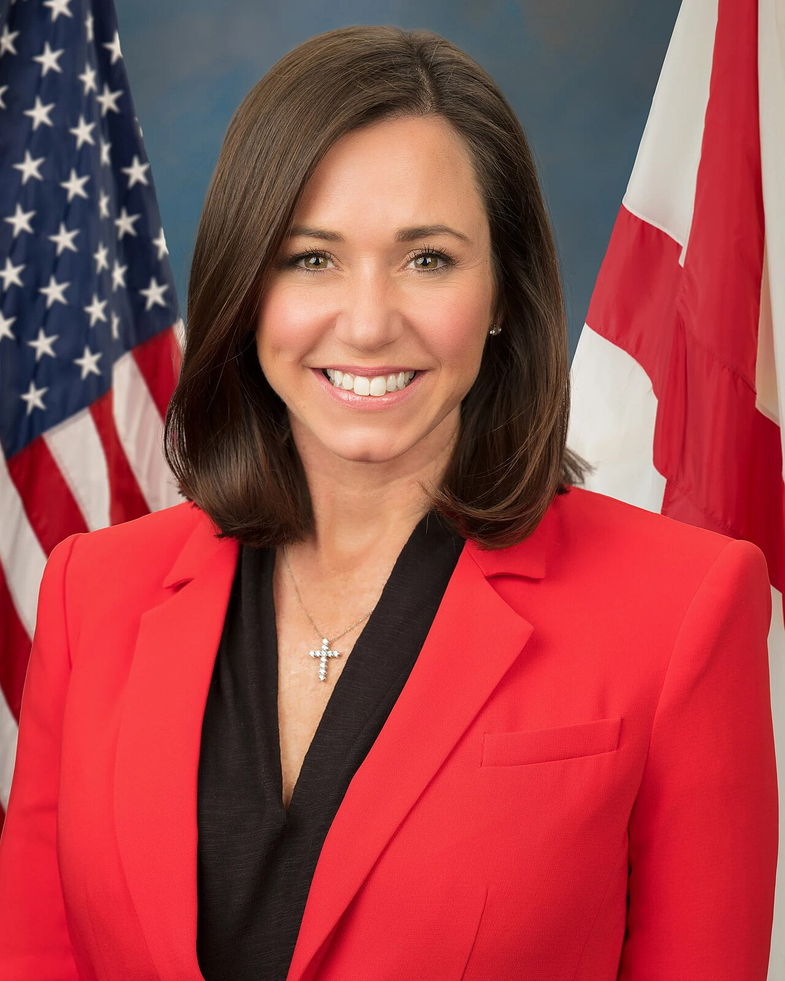
TrackMaggie Goodlander

Co-Sponsor
-
TrackAdam Gray

Co-Sponsor
-
TrackRo Khanna

Co-Sponsor
-
TrackKevin Kiley

Co-Sponsor
-
TrackMichael Lawler

Co-Sponsor
-
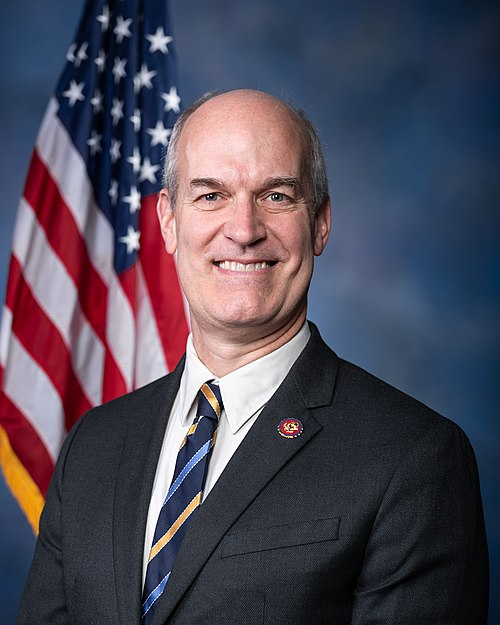
TrackDan Newhouse
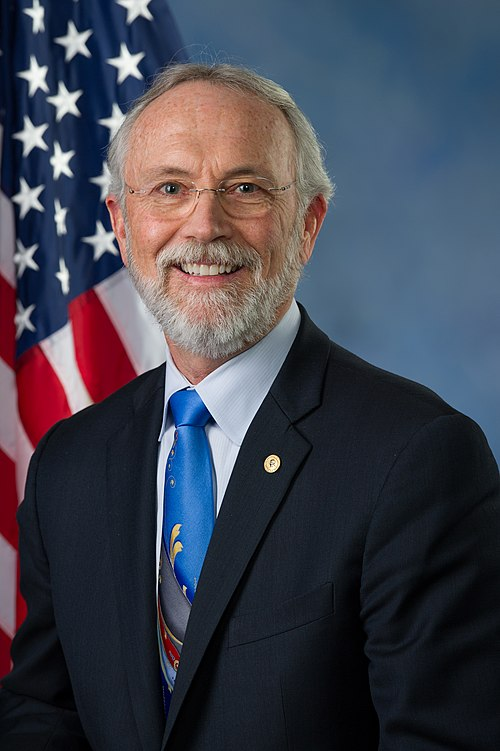
Co-Sponsor
-
TrackZachary Nunn

Co-Sponsor
-
TrackDeborah K. Ross

Co-Sponsor
-
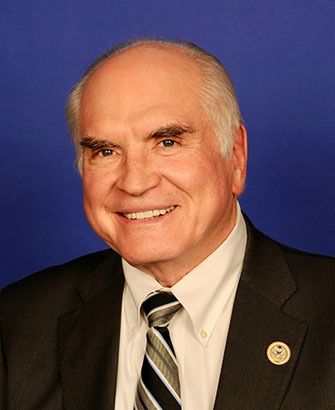
TrackJefferson Van Drew

Co-Sponsor
Actions
2 actions
| Date | Action |
|---|---|
| Nov. 10, 2025 | Introduced in House |
| Nov. 10, 2025 | Referred to the Committee on Ways and Means, and in addition to the Committee on Energy and Commerce, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.