H.R. 5433: Patients Over Profit Act
This bill, known as the Patients Over Profit Act, seeks to address concerns about the ownership structures of health insurance companies and certain healthcare providers, specifically those participating in Medicare. It establishes regulations to prohibit the common ownership of health insurance issuers and providers that offer services under the Medicare program in order to ensure the independence of care provided to patients.
Key Provisions
- Prohibition on Common Ownership: The bill makes it illegal for any individual or entity to simultaneously own or control both a health insurance issuer and an applicable healthcare provider, including those that have management services agreements with these providers.
- Divestment Requirements: Entities that are found to violate the prohibition must divest one of the two holdings—either the health insurance issuer or the applicable provider. For entities acquired before the law is enacted, this divestment must occur within two years. For entities acquired after enactment, it must occur within one year.
- Civil Actions: Various authorities, including the Inspector General of Health and Human Services and state attorneys general, may bring civil actions against violators. Courts can issue orders for compliance and may require the payment of revenue obtained during the period of violation to be deposited into a fund for the community's healthcare needs.
- FTC Review: The Federal Trade Commission (FTC) will review any required divestments to analyze their impact on competition and public interest, and create rules to enforce these provisions.
- Medicare Provisions: Specific amendments are made to Medicare regulations, prohibiting Medicare Advantage plans from contracting with entities that are in violation of these ownership prohibitions. Medicare organizations will have to certify compliance and any false claims submitted by violators will be classified as fraudulent.
Definitions
- Applicable Provider: Entities that receive payment for services covered under Medicare, excluding certain entities like hospitals, durable medical equipment suppliers, and pharmacies.
- Health Insurance Issuer: Defined by existing law, essentially referring to entities involved in providing health insurance coverage.
- Management Services Organization: Organizations providing management or administrative services to applicable providers.
Enforcement and Compliance
The bill authorizes various federal and state officials to enforce compliance and sets forth procedures for how violations will be handled. If someone is found in violation, they are required to cease the conflicting ownership and may face additional financial penalties.
Implementation Timeline
The act will come into effect for Medicare Advantage plans starting from January 1, 2026, setting timelines for compliance and enforcement in alignment with those provisions.
Relevant Companies
- AET (Aetna Inc.): Aetna is a health insurance company that could be affected if found to have overlapping ownership with healthcare providers.
- ANTM (Anthem, Inc.): Anthem could face implications regarding its investment and ownership structures in relation to Medicare providers.
- HUM (Humana Inc.): As a major Medicare Advantage provider, Humana would need to assess its ownership relations to comply with this bill.
- CNC (Centene Corporation): Centene's relationships with healthcare providers may come under scrutiny for compliance with the new ownership rules.
This is an AI-generated summary of the bill text. There may be mistakes.
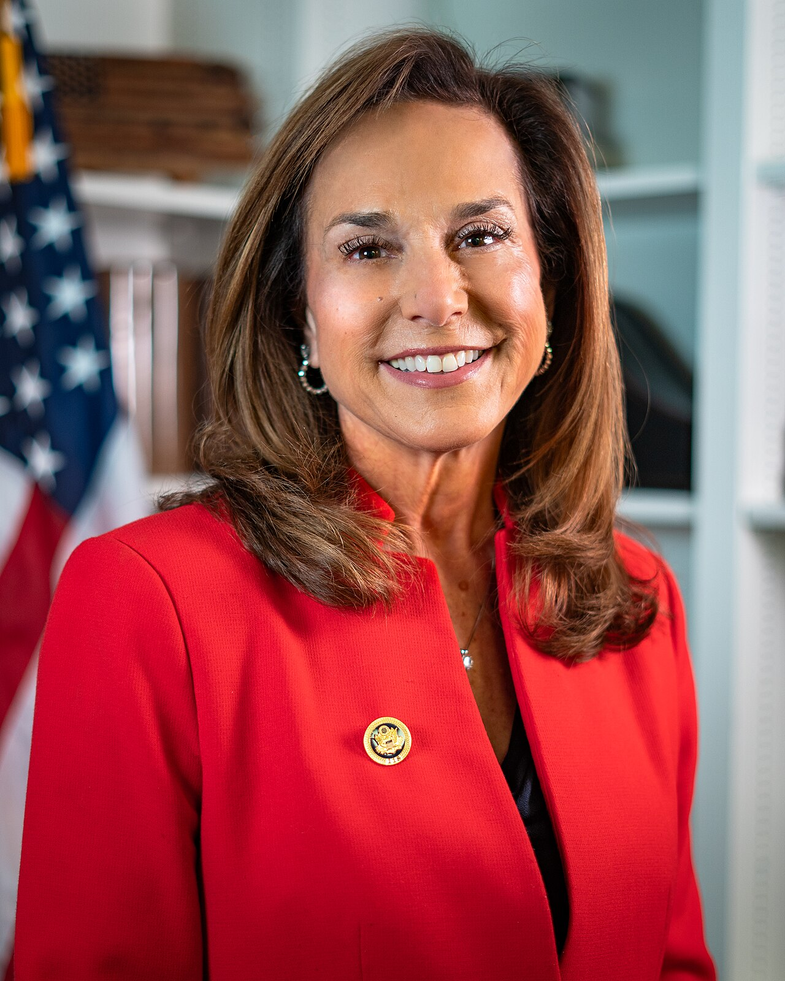
Sponsors
6 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Sep. 17, 2025 | Introduced in House |
| Sep. 17, 2025 | Referred to the Committee on the Judiciary, and in addition to the Committees on Energy and Commerce, and Ways and Means, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.