H.R. 5281: Requiring Enhanced and Accurate Lists of Health Providers Act
This bill, titled the "Requiring Enhanced and Accurate Lists of Health Providers Act" (or "REAL Health Providers Act"), aims to improve the accuracy of provider directories for Medicare Advantage (MA) plans. It sets forth specific requirements for MA organizations to maintain updated and accurate information about healthcare providers available to their enrollees. The main components of the bill include:
Provider Directory Requirements
Starting in 2028, each MA organization offering a specified MA plan must:
- Maintain an Accurate Provider Directory: This directory must be publicly accessible and regularly updated.
- Verification of Provider Information: Provider information must be verified at least once every 90 days. For hospitals or other facilities, verification can occur less frequently but at least once a year.
- Indication of Unverified Providers: If an organization cannot verify a provider's information, it must note that the information may not be current.
- Remove Departed Providers Quickly: Any provider who is no longer part of the plan's network must be removed from the directory within five business days.
Accountability for Directory Accuracy
In regards to cost-sharing and directory accuracy, the bill stipulates that:
- Costs for Non-Participating Providers: If a plan enrollee sees a provider listed in the directory who is actually out-of-network, the enrollee will be responsible for lower out-of-pocket costs, equivalent to what they would have paid had they seen an in-network provider.
- Notifications of Protections: MA organizations must inform enrollees about these cost-sharing protections, ideally at the beginning of annual enrollment periods.
Accuracy Analysis and Reporting
Beginning in 2028, the bill requires annual analyses from MA organizations on the accuracy of their provider directories, including:
- Random sampling of provider information.
- A report of accuracy scores that is submitted to the Secretary of Health and Human Services.
- Public posting of these scores starting in 2029, ensuring transparency about the accuracy of provider directories.
Guidance Issuance
The Secretary of Health and Human Services is tasked with providing guidance for maintaining accurate provider directories, including:
- Best practices for updating provider directories.
- Information on data sources for maintaining directory accuracy.
- Guidance for providers on updating their information in relevant systems.
Funding Provisions
The bill allocates $4 million for fiscal year 2026 specifically for the implementation of the new requirements.
GAO Study and Reporting Mandate
The Government Accountability Office (GAO) is directed to study the implementation of these new provisions and report their findings by January 2032, focusing on cost-sharing protections and accuracy in provider information.
Enforcement and Compliance
MA organizations will be subject to scrutiny to ensure compliance with directory accuracy and reporting requirements.
Relevant Companies
- MRNA (Moderna, Inc.) - As a major healthcare provider, changes in how provider information is handled could impact their operational logistics and patient interactions.
- CI (Cigna Corporation) - As a health insurance provider, Cigna will need to adjust their practices to meet the new directory accuracy requirements.
- UNH (UnitedHealth Group Incorporated) - Similar to Cigna, UnitedHealth must adapt to compliance with the enhanced provider directory accuracy standards.
This is an AI-generated summary of the bill text. There may be mistakes.
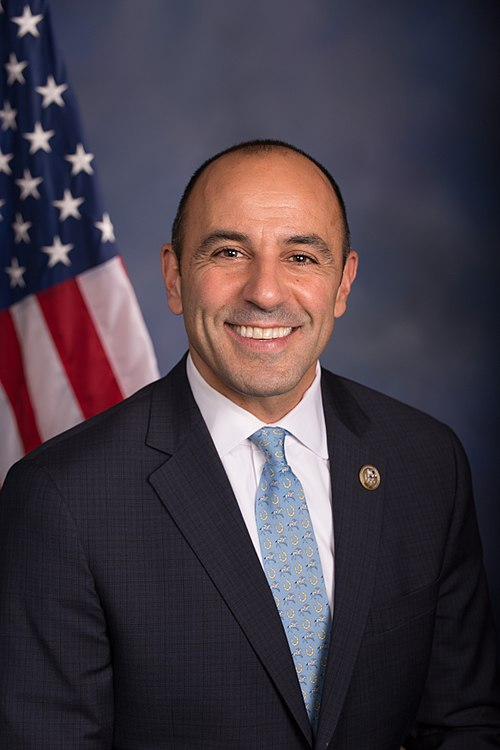
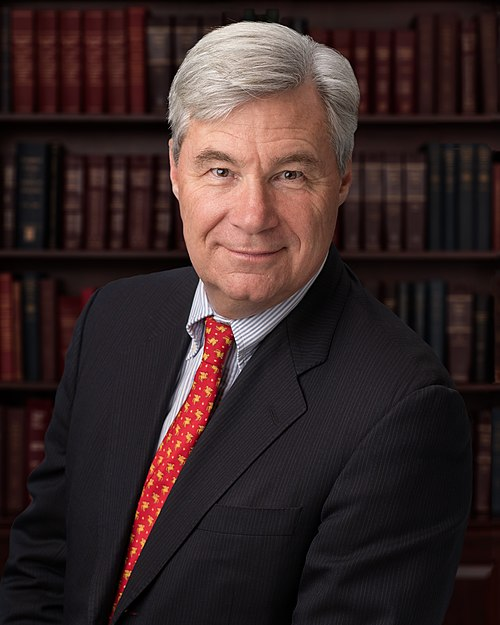
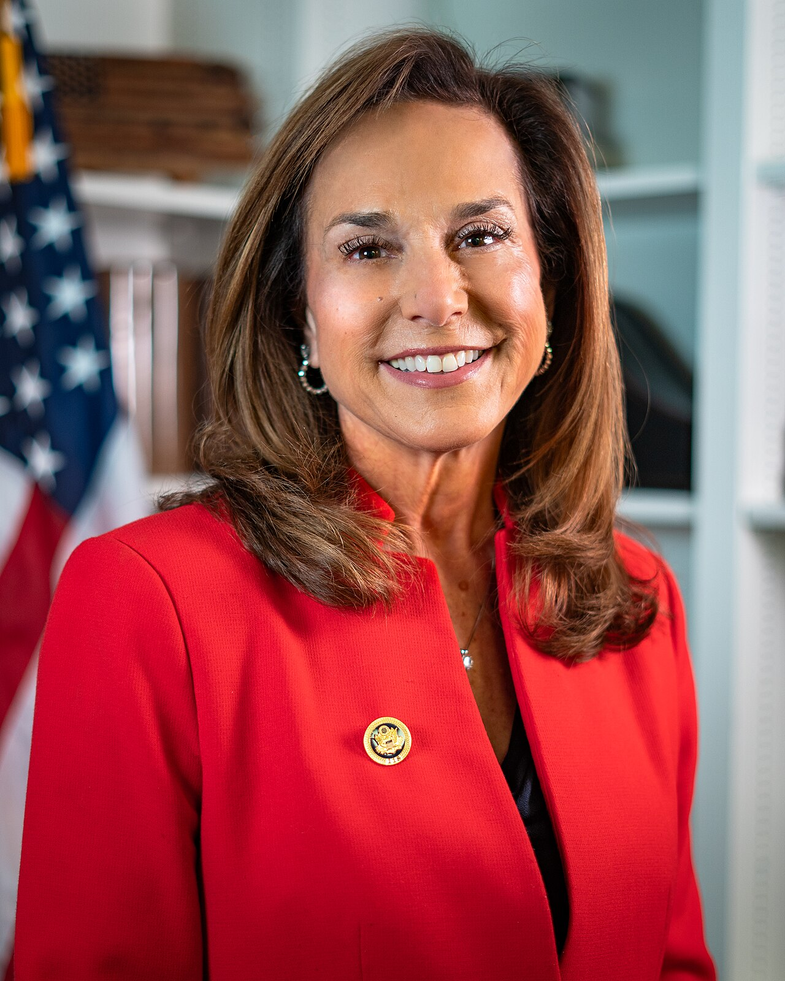
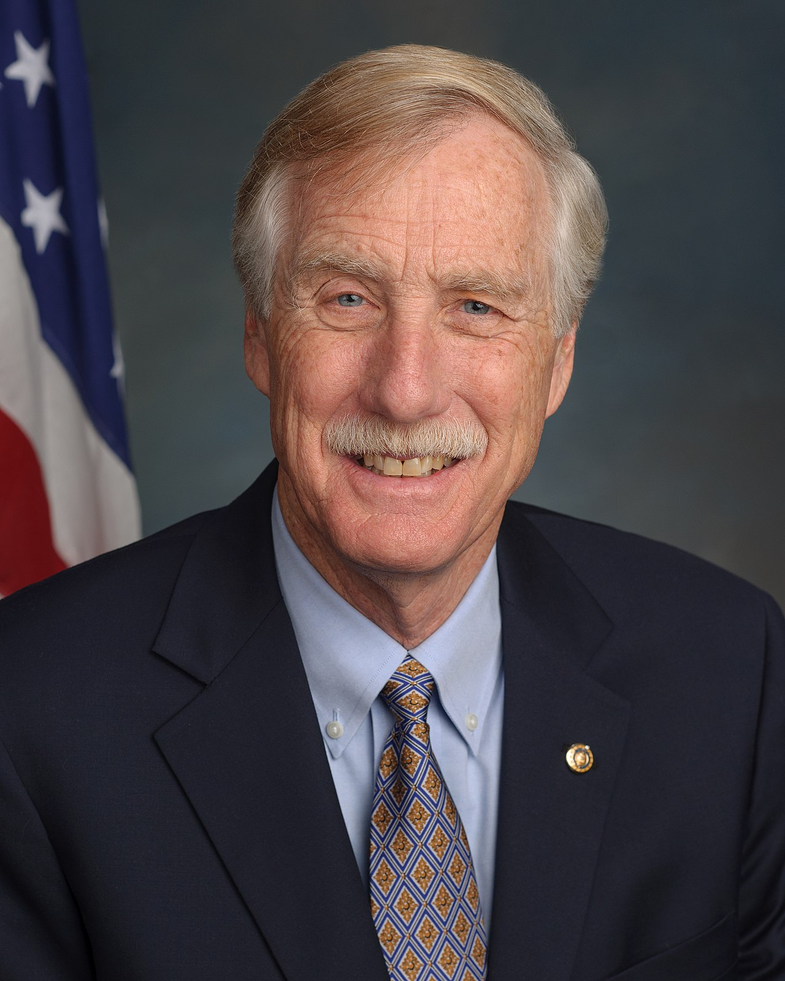
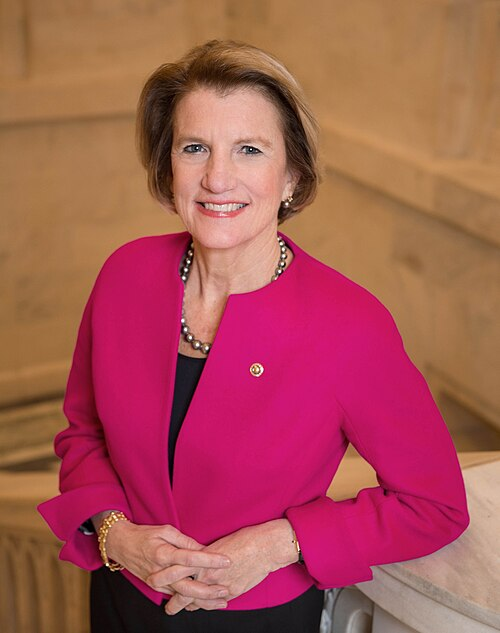
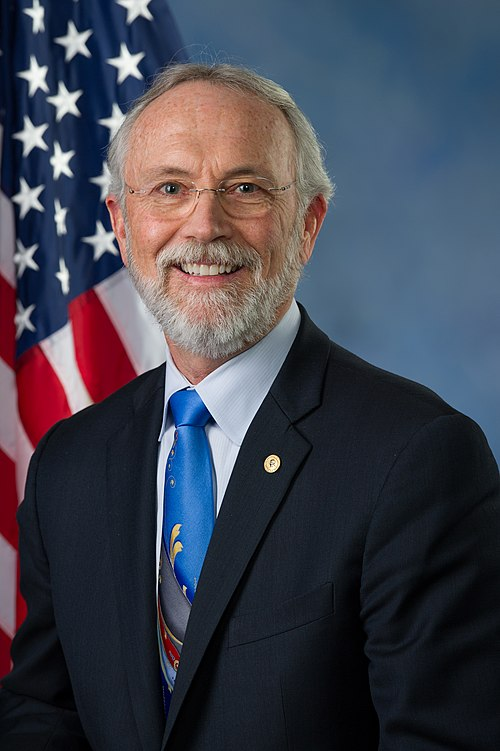
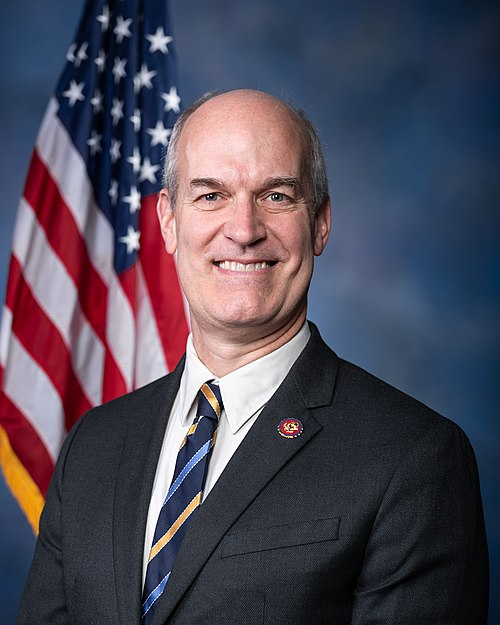
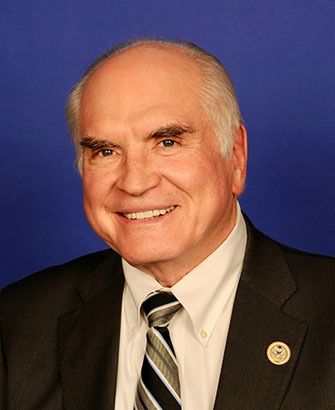
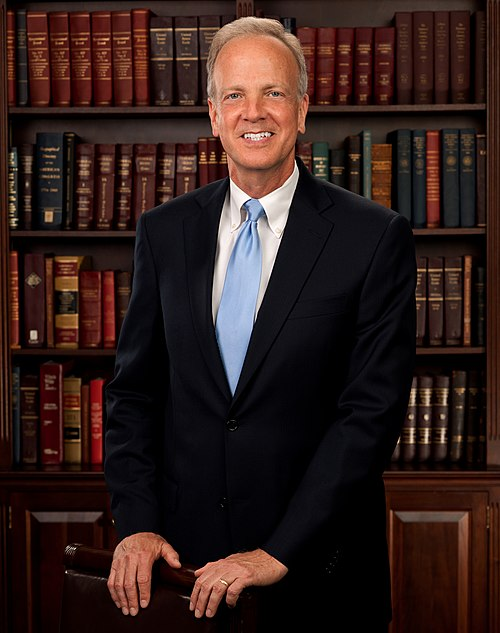
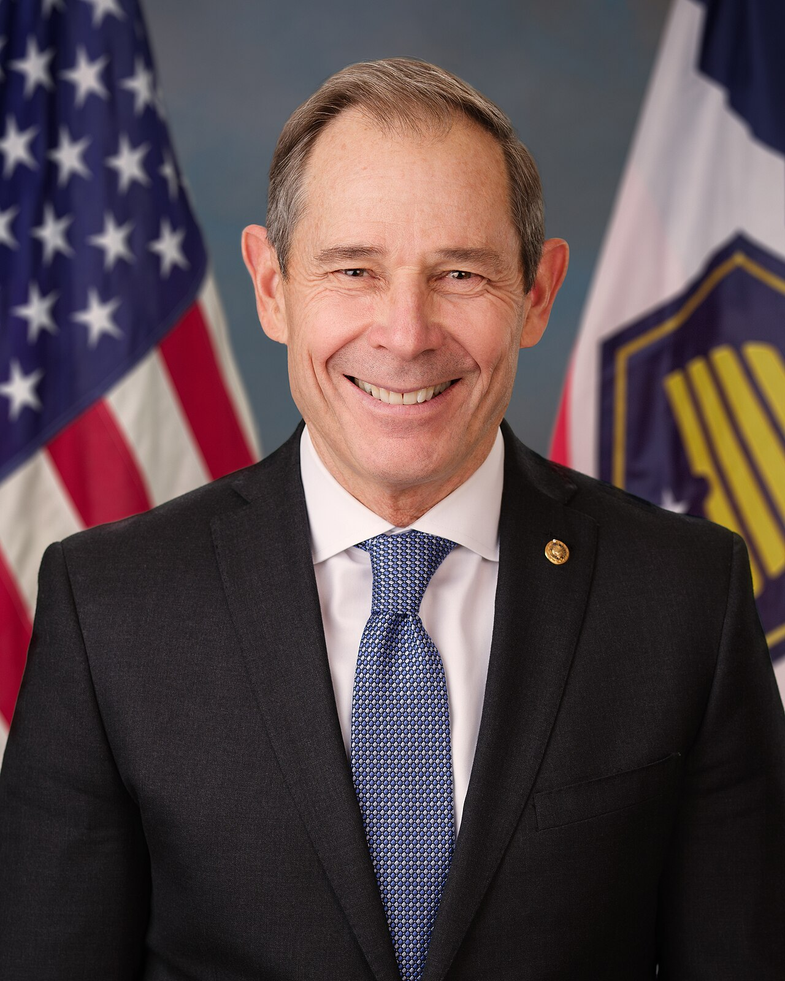
Sponsors
6 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Sep. 10, 2025 | Introduced in House |
| Sep. 10, 2025 | Referred to the Committee on Ways and Means, and in addition to the Committee on Energy and Commerce, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.