H.R. 5243: To amend title XVIII of the Social Security Act to increase data transparency for supplemental benefits under Medicare Advantage.
This bill proposes changes to the Social Security Act that would enhance data transparency for supplemental benefits provided under Medicare Advantage plans starting January 1, 2029. Here are the key components of the bill:
Mandatory Reporting of Supplemental Benefits
The bill requires Medicare Advantage (MA) organizations to submit detailed data on supplemental benefits for each enrollee. This data will include:
- Eligibility for supplemental benefits
- Types of benefit categories offered
- Utilization of these benefits
- Payments for these benefits, including total amounts spent by plans per enrollee and out-of-pocket costs per enrollee per use
Annual Data Access and Publication
Beginning in 2030, the Secretary of Health and Human Services (HHS) will make the reported data available annually to the public and other interested parties. This will facilitate:
- Evaluations and analyses supporting the Medicare Advantage program
- Health care-related research
Additionally, a public data file will be published on the internet by October 1 each year that includes the submissions from MA organizations.
Safeguarding Privacy
The bill stipulates that any data released will protect the privacy of individuals. The Secretary will implement measures to ensure that information related to individual enrollees remains confidential.
Consistency with Existing Regulations
The bill clarifies that its provisions do not interfere with existing information collection efforts, as specified in a prior notice from the Federal Register dated March 14, 2023.
Overall Impact
The bill aims to improve transparency in how supplemental benefits are managed within Medicare Advantage plans, allowing for better evaluation and understanding of these benefits, while also ensuring the protection of individual privacy.
Relevant Companies
- ANTM (Anthem, Inc.): This bill could impact Anthem as they are a major provider of Medicare Advantage plans, requiring them to adapt to new data reporting requirements.
- HUM (Humana Inc.): As a significant player in the Medicare Advantage market, Humana will also be required to comply with the new data reporting mandates.
- CNC (Centene Corporation): Centene offers Medicare Advantage plans and would need to align its reporting practices with the new transparency requirements.
This is an AI-generated summary of the bill text. There may be mistakes.
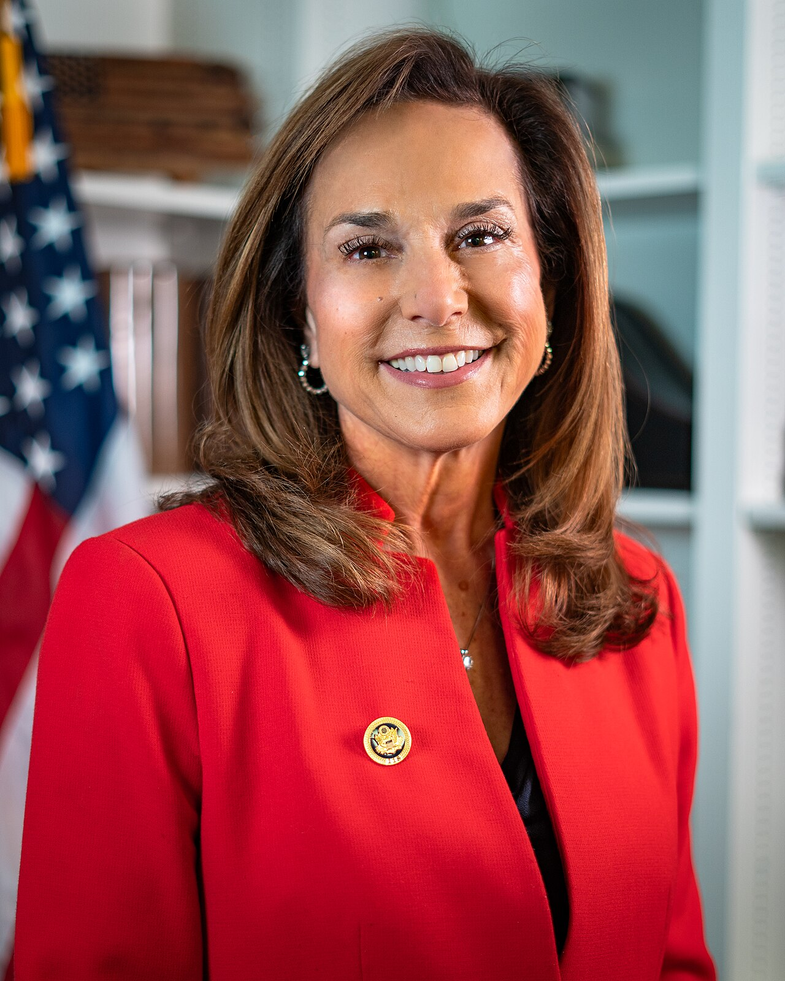
Sponsors
1 sponsor
Actions
2 actions
| Date | Action |
|---|---|
| Sep. 10, 2025 | Introduced in House |
| Sep. 10, 2025 | Referred to the Committee on Ways and Means, and in addition to the Committee on Energy and Commerce, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.