H.R. 4710: No Surprises Act Enforcement Act
This bill, titled the No Surprises Act Enforcement Act, aims to enhance the enforcement of existing regulations surrounding balance billing practices in healthcare. Balance billing occurs when a healthcare provider bills a patient for the difference between what the patient's insurance pays and what the provider charges. The bill focuses on the following key areas:
1. Increasing Penalties for Violations
The bill proposes to increase penalties for group health plans and health insurance issuers that violate balance billing requirements. Specifically:
- It introduces a new civil penalty of up to $10,000 for each failure to comply with certain balance billing provisions outlined in the Public Health Service Act (PHSA), the Employee Retirement Income Security Act (ERISA), and the Internal Revenue Code (IRC).
- This penalty is over and above an existing $100 per day fine, which remains in place for other violations.
2. Penalties for Late Payments
The legislation also establishes additional penalties for late or non-payments after determinations made by independent dispute resolution (IDR) entities:
- Plans and providers that fail to make timely payments will incur an additional charge of three times the difference between the initial payment and the out-of-network rate for that service.
- Interest will be applied to any overdue amounts, with further clarification on the specifics left to the Secretary of Health and Human Services.
3. Transparency Reporting Requirements
To enhance oversight and accountability, the bill mandates annual and semi-annual reporting requirements:
- The Secretary of Health and Human Services must report to Congress on audits of health plans and any enforcement actions taken against them.
- These reports will include the number of audits conducted, complaints received from providers and patients, civil monetary penalties imposed, and non-monetary corrective actions taken.
4. Enhanced Compliance Measures
The bill strengthens compliance measures by ensuring that plans and nonparticipating providers submit notifications of required payments as outlined by the Secretary of Health and Human Services. This aims to streamline processes and improve accountability in the healthcare payment system.
Relevant Companies
- UNH (UnitedHealth Group): As one of the largest health insurance providers, this bill could impact its balance billing practices and financial penalties for non-compliance.
- ANTM (Anthem, Inc.): Involved in providing health insurance, stricter enforcement could affect their operations regarding payment resolutions and balance billing.
- CNC (Centene Corporation): As a major provider of healthcare plans, increased penalties could impact Centene's compliance costs and operational practices.
This is an AI-generated summary of the bill text. There may be mistakes.
Sponsors
15 bill sponsors
-
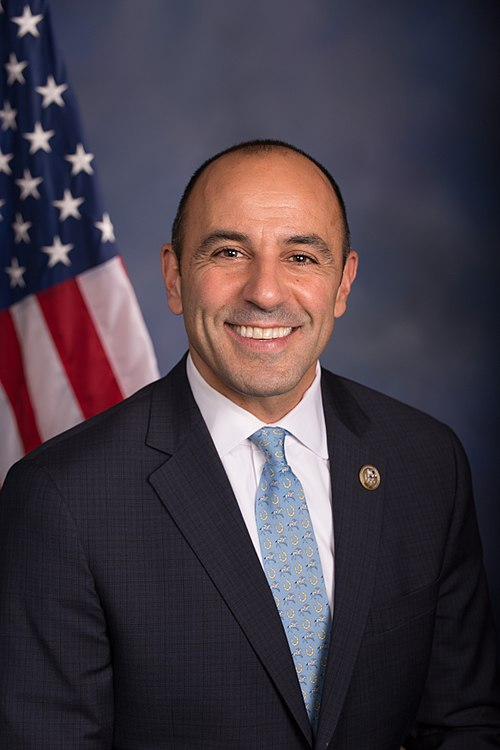
TrackGregory F. Murphy

Sponsor
-
TrackHerbert Conaway
Co-Sponsor
-
TrackNeal P. Dunn
Co-Sponsor
-
TrackAndy Harris
Co-Sponsor
-
TrackJohn Joyce

Co-Sponsor
-
TrackMichael Lawler

Co-Sponsor
-
TrackNathaniel Moran

Co-Sponsor
-
TrackJoseph D. Morelle

Co-Sponsor
-
TrackRobert Onder
Co-Sponsor
-
TrackJimmy Panetta
Co-Sponsor
-
TrackRaul Ruiz

Co-Sponsor
-
TrackKim Schrier

Co-Sponsor
-
TrackThomas R. Suozzi
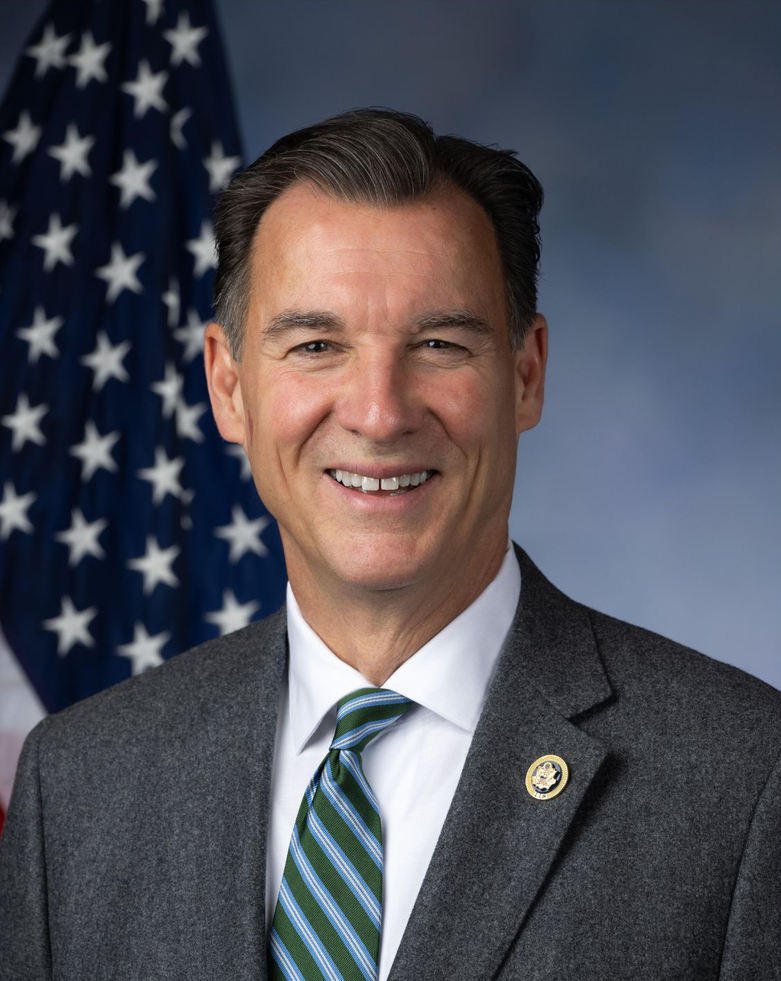
Co-Sponsor
-
TrackBeth Van Duyne

Co-Sponsor
-
TrackEugene Vindman

Co-Sponsor
Actions
2 actions
| Date | Action |
|---|---|
| Jul. 23, 2025 | Introduced in House |
| Jul. 23, 2025 | Referred to the Committee on Energy and Commerce, and in addition to the Committees on Education and Workforce, and Ways and Means, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.