H.R. 3907: Expand Navigators’ Resources for Outreach, Learning, and Longevity Act of 2025
This bill, known as the *Expand Navigators’ Resources for Outreach, Learning, and Longevity Act of 2025* (or ENROLL Act of 2025), aims to amend the Patient Protection and Affordable Care Act (ACA) to enhance the navigator program that helps individuals understand and access health insurance options. Here are the key changes proposed by the bill:
1. Selection of Navigator Recipients
The bill provides for new criteria in selecting which entities receive grants to serve as navigators. Specifically:
- Entities will be chosen based on their ability to perform specific duties, rather than whether they provide information on non-qualified health plans.
- At least one of the entities awarded a grant each year must be a community and consumer-focused nonprofit organization.
2. Expanded Responsibilities of Navigators
Navigators will have expanded responsibilities to assist consumers:
- The definition of the information navigators must provide is broadened to include not just qualified health plans but also State Medicaid plans and State children’s health insurance programs.
- Navigators will be required to conduct public education in plain language about health insurance options and protections.
- These duties can be performed at any time during the year, not just during open enrollment.
3. Requirements for Physical Presence
The bill mandates that navigator entities must maintain a physical presence in the state of the exchange, ensuring that consumers have access to in-person assistance when needed.
4. Funding Provisions
The bill outlines new funding mechanisms:
- Grants for navigators will be provided from federal and state exchanges, ensuring adequate resources are allocated for implementation.
- For federal exchanges, it specifies that $100 million must be allocated each year from user fees collected from participating health insurance issuers, starting from fiscal year 2026. This amount will remain available until fully spent.
5. Implementation Timeline
The changes proposed in this bill would take effect for plan years beginning on or after January 1, 2026.
Relevant Companies
- UNH - UnitedHealth Group: As a major player in the health insurance market, changes in navigator program requirements and increased outreach could affect their enrollment numbers and overall market strategies.
- ANTM - Anthem, Inc.: Similar to UnitedHealth Group, changes in how navigators operate could influence how customers access their plans and affect enrollment rates.
- CNC - Centene Corporation: As a provider of Medicaid and health plans, they could see changes in how consumers access their services due to the expanded responsibilities of navigators.
This is an AI-generated summary of the bill text. There may be mistakes.
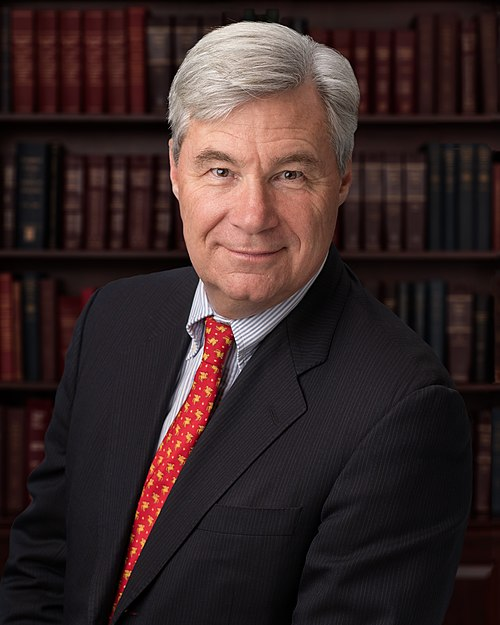
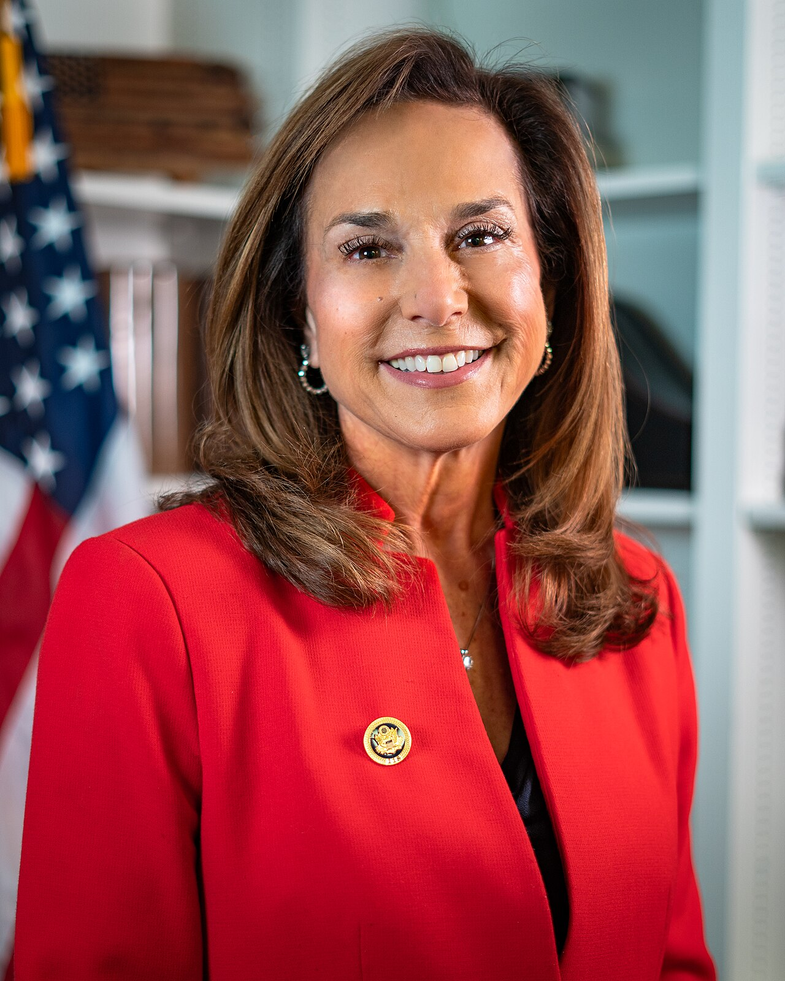
Sponsors
2 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Jun. 11, 2025 | Introduced in House |
| Jun. 11, 2025 | Referred to the House Committee on Energy and Commerce. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.