H.R. 3277: Ensuring Lasting Smiles Act
This bill, titled the Ensuring Lasting Smiles Act
, aims to improve healthcare coverage for those affected by congenital anomalies or birth defects. Here are the main points of the bill:
Health Insurance Requirements
The bill requires that group health plans and health insurance issuers provide coverage for both outpatient and inpatient services related to diagnosing and treating congenital anomalies or birth defects that primarily affect the eyes, ears, teeth, mouth, or jaw. This includes the following:
- Items and services necessary to improve, repair, or restore function or appearance, determined to be medically necessary by a treating physician.
- Treatment for any missing or abnormal body parts, including services that address complications from prior treatments.
- Supportive dental, orthodontic, or prosthetic services from birth until the medical or surgical intervention has been completed, including any follow-up treatments needed.
Financial Requirements
The coverage for these services may involve cost-sharing, such as copayments and deductibles, although these must not be more restrictive than those applied to other medical or surgical benefits in the plan.
Exclusions
The required coverage does not include cosmetic surgery that is not linked to a medically determined congenital anomaly or birth defect. This means any procedures undertaken solely for aesthetic purposes unrelated to medical necessity are excluded from coverage.
Notice Requirements
By January 1, 2026, group health plans and insurance issuers must inform all participants and beneficiaries about this coverage in their documents detailing available services.
Definitions
The bill defines a congenital anomaly or birth defect
as any structural or functional anomaly that occurs during pregnancy, which can be caused by a range of genetic and environmental factors and can affect individuals in various ways such as:
- Being evident at birth or developing later in life.
- Manifesting as abnormal anatomical structures.
- Causing physical, sensory, or cognitive disabilities.
- Leading to syndromes, diseases, or other health problems.
Studies and Reports
The Secretary of Health and Human Services is tasked with conducting a study by December 31, 2027, to evaluate how accessible the necessary healthcare services are under these coverage requirements. The study will assess:
- The adequacy of networks of providers for these services.
- Changes in patients' out-of-pocket costs for affected procedures and overall costs for services associated with congenital anomalies or birth defects.
Implementation Timeline
The provisions of this bill will take effect for plan years beginning on or after January 1, 2026.
Relevant Companies
- UNH (UnitedHealth Group): As a major health insurer, UnitedHealth Group will need to adjust its coverage policies to comply with the new requirements, potentially affecting its cost structures and service offerings.
- ANTM (Anthem Inc.): Similar to UnitedHealth, Anthem will have to implement changes in its health plans to provide the mandated coverage, which could involve increased administrative processes and modifications in claims handling.
- CNC (Centene Corporation): Centene, which provides managed care services, will need to adapt its health plans to ensure coverage for congenital anomalies and might face financial implications based on the new coverage requirements.
This is an AI-generated summary of the bill text. There may be mistakes.
Sponsors
110 bill sponsors
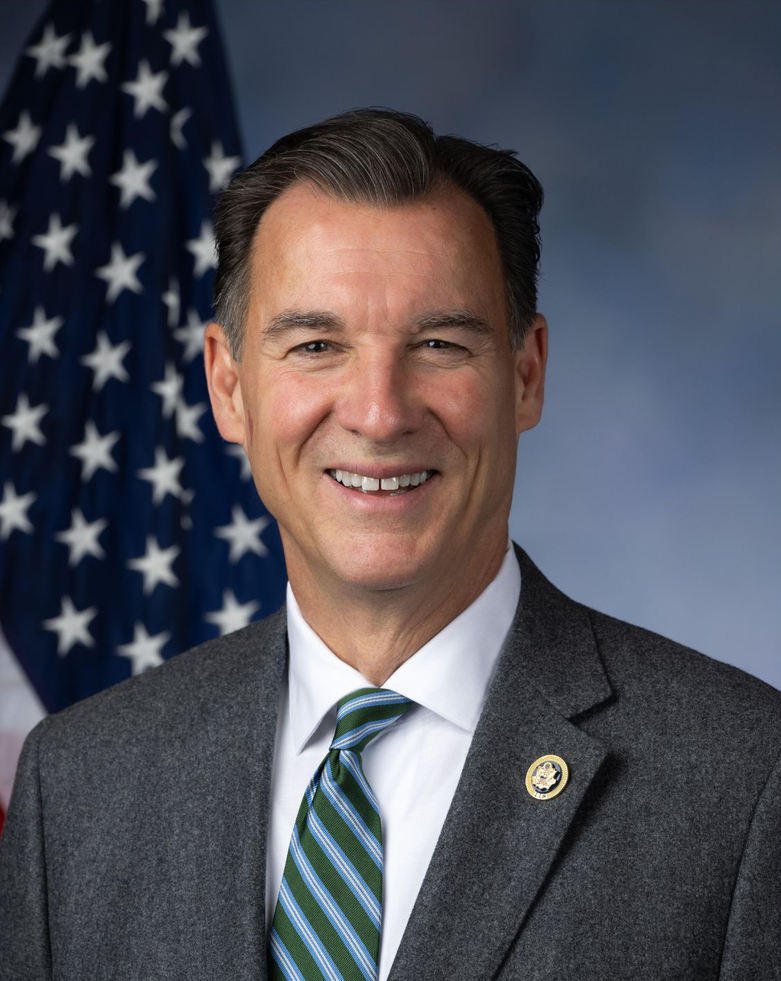
-
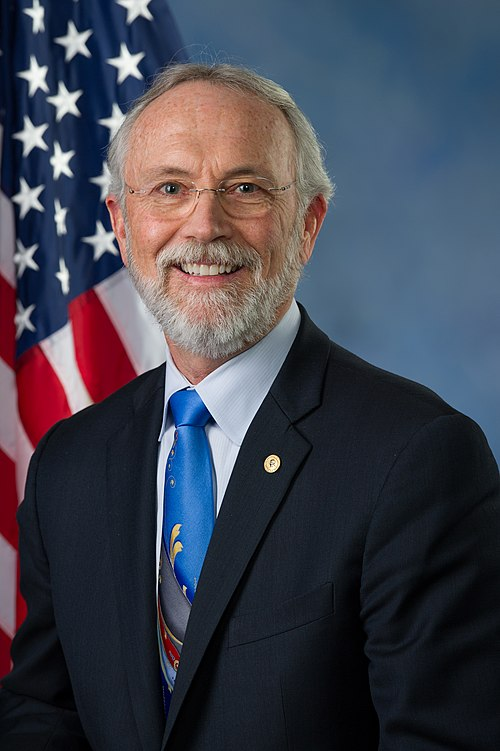
TrackNeal P. Dunn
Sponsor
-
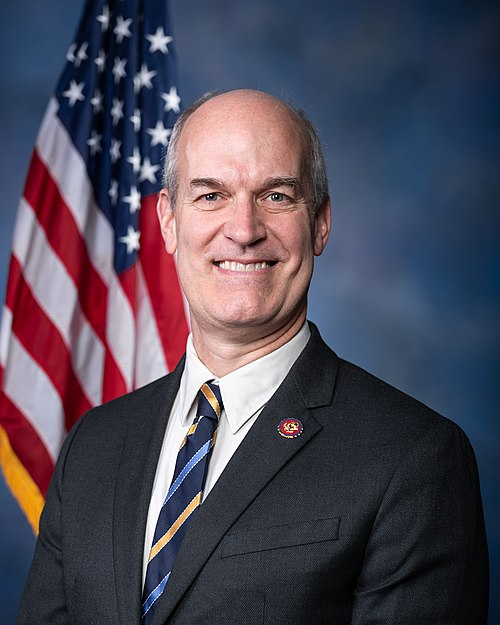
TrackRobert B. Aderholt
Co-Sponsor
-
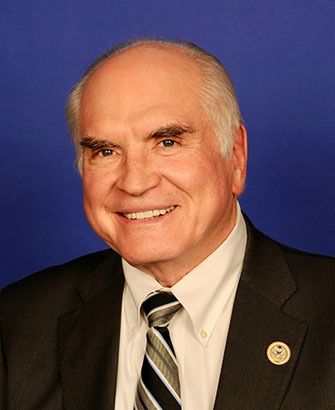
TrackGabe Amo

Co-Sponsor
-
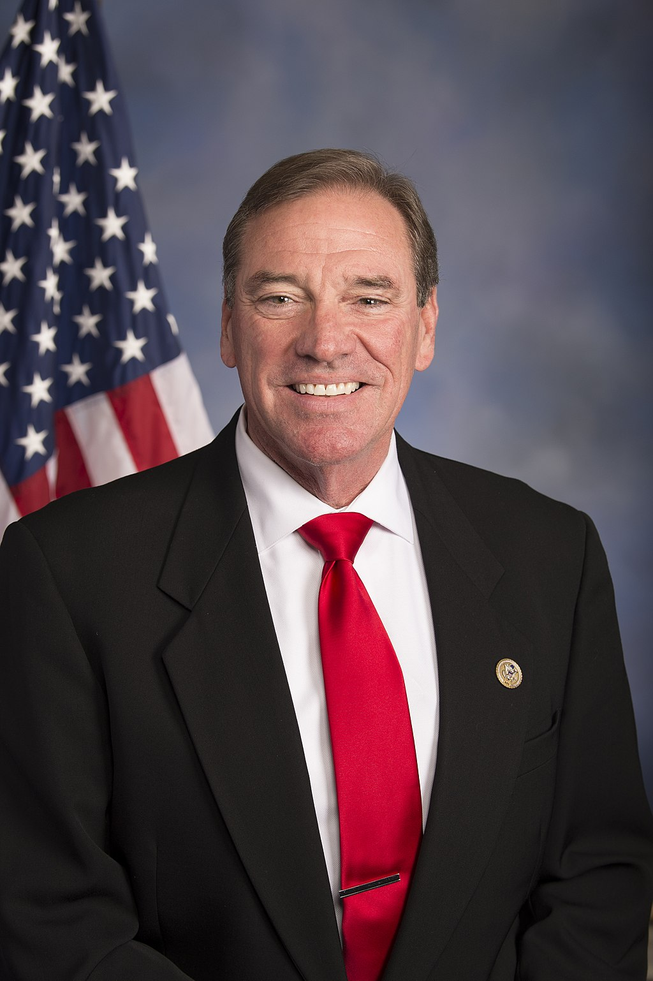
TrackJake Auchincloss

Co-Sponsor
-
TrackBrian Babin

Co-Sponsor
-
TrackBecca Balint

Co-Sponsor
-
TrackAndy Barr

Co-Sponsor
-
TrackMichael Baumgartner

Co-Sponsor
-
TrackNicholas Begich

Co-Sponsor
-
TrackAmi Bera

Co-Sponsor
-
TrackJack Bergman

Co-Sponsor
-
TrackDonald S. Beyer, Jr.
Co-Sponsor
-
TrackGus M. Bilirakis
Co-Sponsor
-
TrackSuzanne Bonamici
Co-Sponsor
-
TrackMike Bost

Co-Sponsor
-
TrackRobert Bresnahan

Co-Sponsor
-
TrackJulia Brownley

Co-Sponsor
-
TrackJanelle Bynum

Co-Sponsor
-
TrackKathy Castor

Co-Sponsor
-
TrackJoaquin Castro

Co-Sponsor
-
TrackSheila Cherfilus-McCormick

Co-Sponsor
-
TrackJudy Chu

Co-Sponsor
-
TrackEmanuel Cleaver
Co-Sponsor
-
TrackAngie Craig
Co-Sponsor
-
TrackSharice Davids

Co-Sponsor
-
TrackDonald G. Davis

Co-Sponsor
-
TrackRosa L. DeLauro

Co-Sponsor
-
TrackSuzan K. DelBene

Co-Sponsor
-
TrackDebbie Dingell

Co-Sponsor
-
TrackSarah Elfreth

Co-Sponsor
-
TrackCleo Fields

Co-Sponsor
-
TrackRandy Fine

Co-Sponsor
-
TrackScott Fitzgerald
Co-Sponsor
-
TrackBrian K. Fitzpatrick

Co-Sponsor
-
TrackValerie P. Foushee

Co-Sponsor
-
TrackLois Frankel
Co-Sponsor
-
TrackScott Franklin

Co-Sponsor
-
TrackJohn Garamendi

Co-Sponsor
-
TrackCarlos A. Gimenez
Co-Sponsor
-
TrackDaniel S. Goldman

Co-Sponsor
-
TrackPaul A. Gosar

Co-Sponsor
-
TrackJosh Gottheimer

Co-Sponsor
-
TrackGlenn Grothman

Co-Sponsor
-
TrackJosh Harder

Co-Sponsor
-
TrackAndy Harris
Co-Sponsor
-
TrackJames A. Himes
Co-Sponsor
-
TrackAshley Hinson

Co-Sponsor
-
TrackChrissy Houlahan

Co-Sponsor
-
TrackVal T. Hoyle

Co-Sponsor
-
TrackGlenn Ivey
Co-Sponsor
-
TrackPramila Jayapal

Co-Sponsor
-
TrackJulie Johnson

Co-Sponsor
-
TrackRobin L. Kelly
Co-Sponsor
-
TrackRo Khanna

Co-Sponsor
-
TrackYoung Kim
Co-Sponsor
-
TrackRaja Krishnamoorthi

Co-Sponsor
-
TrackGreg Landsman

Co-Sponsor
-
TrackNicholas A. Langworthy
Co-Sponsor
-
TrackMike Levin

Co-Sponsor
-
TrackStephen F. Lynch

Co-Sponsor
-
TrackSeth Magaziner

Co-Sponsor
-
TrackNicole Malliotakis

Co-Sponsor
-
TrackJohn Mannion

Co-Sponsor
-
TrackDoris O. Matsui

Co-Sponsor
-
TrackSarah McBride

Co-Sponsor
-
TrackApril McClain Delaney

Co-Sponsor
-
TrackJames P. McGovern

Co-Sponsor
-
TrackDaniel Meuser

Co-Sponsor
-
TrackKweisi Mfume

Co-Sponsor
-
TrackMariannette Miller-Meeks
Co-Sponsor
-
TrackDave Min
Co-Sponsor
-
TrackGwen Moore

Co-Sponsor
-
TrackFrank J. Mrvan

Co-Sponsor
-
TrackGregory F. Murphy

Co-Sponsor
-
TrackJoe Neguse

Co-Sponsor
-
TrackTroy E. Nehls

Co-Sponsor
-
TrackEleanor Holmes Norton

Co-Sponsor
-
TrackZachary Nunn

Co-Sponsor
-
TrackJohnny Olszewski

Co-Sponsor
-
TrackIlhan Omar

Co-Sponsor
-
TrackBurgess Owens

Co-Sponsor
-
TrackJimmy Panetta
Co-Sponsor
-
TrackChris Pappas

Co-Sponsor
-
TrackMarie Gluesenkamp Perez

Co-Sponsor
-
TrackBrittany Pettersen

Co-Sponsor
-
TrackMark Pocan
Co-Sponsor
-
TrackMike Quigley

Co-Sponsor
-
TrackJamie Raskin

Co-Sponsor
-
TrackDeborah K. Ross

Co-Sponsor
-
TrackJohn H. Rutherford
Co-Sponsor
-
TrackPatrick Ryan

Co-Sponsor
-
TrackMaria Elvira Salazar
Co-Sponsor
-
TrackAndrea Salinas
Co-Sponsor
-
TrackDerek Schmidt
Co-Sponsor
-
TrackKim Schrier

Co-Sponsor
-
TrackTerri A. Sewell

Co-Sponsor
-
TrackLateefah Simon

Co-Sponsor
-
TrackMichael K. Simpson
Co-Sponsor
-
TrackDarren Soto

Co-Sponsor
-
TrackGreg Stanton

Co-Sponsor
-
TrackMarilyn Strickland

Co-Sponsor
-
TrackThomas R. Suozzi
Co-Sponsor
-
TrackRashida Tlaib

Co-Sponsor
-
TrackJill N. Tokuda

Co-Sponsor
-
TrackJefferson Van Drew

Co-Sponsor
-
TrackEugene Vindman

Co-Sponsor
-
TrackJames R. Walkinshaw

Co-Sponsor
-
TrackDebbie Wasserman Schultz
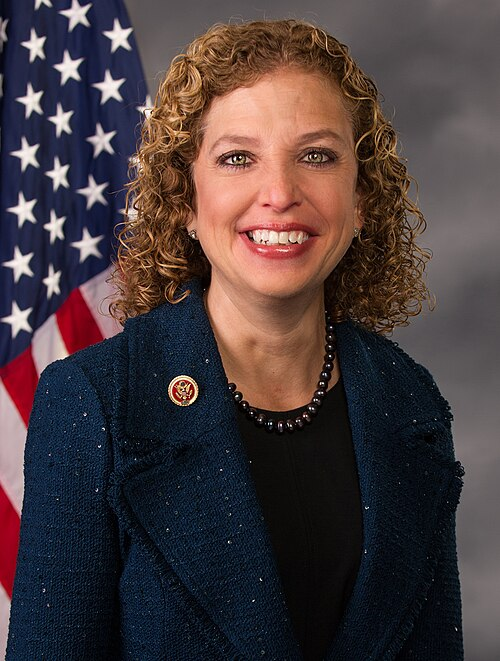
Co-Sponsor
-
TrackRobert J. Wittman

Co-Sponsor
-
TrackRudy Yakym III

Co-Sponsor
Actions
2 actions
| Date | Action |
|---|---|
| May. 08, 2025 | Introduced in House |
| May. 08, 2025 | Referred to the Committee on Energy and Commerce, and in addition to the Committees on Education and Workforce, and Ways and Means, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.