S. 526: Pharmacy Benefit Manager Transparency Act of 2025
This bill, known as the Pharmacy Benefit Manager Transparency Act of 2025, aims to increase transparency and prevent unfair practices in the pharmacy benefit management (PBM) industry, which plays a significant role in determining the costs and reimbursements for prescription drugs. Here are the key provisions outlined in the bill:
1. Prohibition on Unfair Practices
The bill prohibits PBMs from engaging in certain behaviors that could be deemed unfair or deceptive in their pricing of prescription drugs. Specifically, it restricts PBMs from:
- Charging health plans more for a drug than they reimburse pharmacies, while keeping the difference.
- Reducing or rescinding reimbursements to pharmacies without justified reasons.
- Increasing fees or lowering reimbursements to offset government-mandated changes.
2. Conditions for Exceptions
There are exceptions to these prohibitions if the PBM:
- Passes on 100% of any discounts or rebates to the health plan or payer.
- Provides full disclosure of drug costs and any fees charged to health plans and pharmacies.
- Discloses any payments they receive from drug manufacturers.
3. Reporting Requirements
PBMs must report to the relevant federal authorities on a yearly basis. This includes:
- The total difference between what they are paid by health plans and what they pay to pharmacies.
- Details on fees charged to pharmacies and any reimbursement changes made over the year.
- Justifications for any changes in how drugs are classified in terms of costs to consumers.
4. Protection of Information
Any disclosure made under this act must not include personally identifiable information about patients or their doctors.
5. Whistleblower Protections
The bill establishes protections for individuals who report violations of the law related to PBM activities. This includes prohibiting retaliation against individuals who assist law enforcement or provide information about potential violations.
6. Enforcement
Enforcement of the bill will be conducted by the Federal Trade Commission (FTC) and state attorneys general, who can initiate civil actions if they believe the law is being violated. Violations can lead to significant penalties, including fines that could reach up to $1 million.
7. Transparency Enhancements
The bill emphasizes the need for greater transparency regarding the operations and business practices of PBMs. This includes the requirement for PBMs to disclose payment structures and how drug pricing affects health plans and consumers.
Relevant Companies
- CVS: As a major pharmacy benefit manager, CVS could face changes in its operational practices and pricing structures.
- UnitedHealth Group: This company operates one of the largest PBMs and may need to adjust its reimbursement models to comply with the new regulations.
- Elan Corporation: As a pharmaceutical company, Elan may see impacts on its relationships with PBMs regarding drug pricing and reimbursement practices.
This is an AI-generated summary of the bill text. There may be mistakes.
Sponsors
15 bill sponsors
-
TrackChuck Grassley
Sponsor
-
TrackJohn Boozman

Co-Sponsor
-
TrackMaria Cantwell

Co-Sponsor
-
TrackShelley Moore Capito
Co-Sponsor
-
TrackJoni Ernst
Co-Sponsor
-
TrackRuben Gallego

Co-Sponsor
-
TrackMartin Heinrich

Co-Sponsor
-
TrackCindy Hyde-Smith

Co-Sponsor
-
TrackRoger Marshall

Co-Sponsor
-
TrackJerry Moran
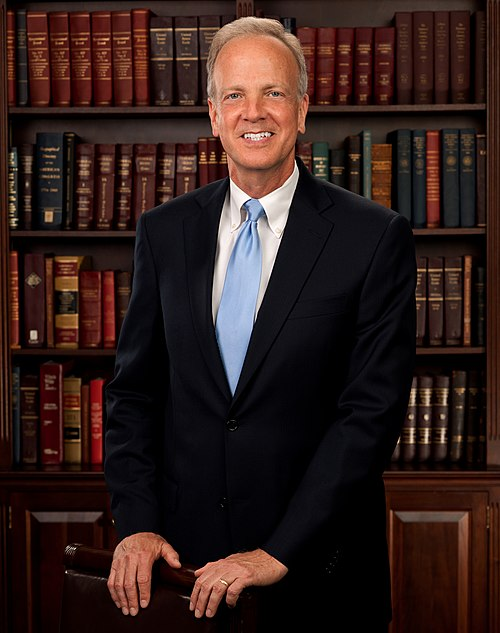
Co-Sponsor
-
TrackMike Rounds

Co-Sponsor
-
TrackJeanne Shaheen
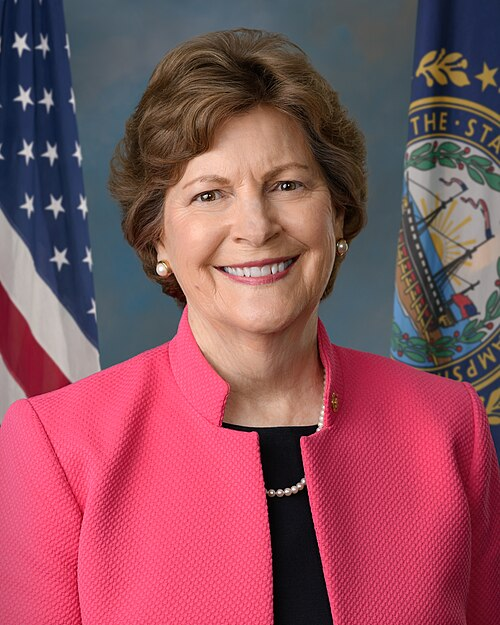
Co-Sponsor
-
TrackThom Tillis

Co-Sponsor
-
TrackRaphael G. Warnock
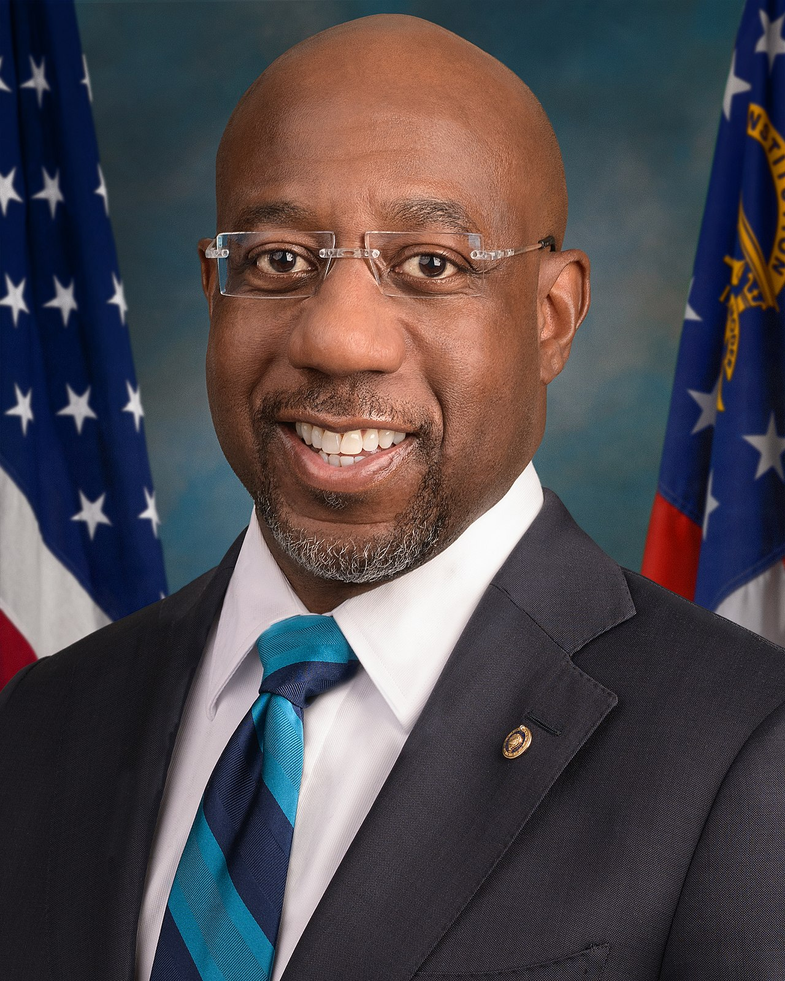
Co-Sponsor
-
TrackPeter Welch
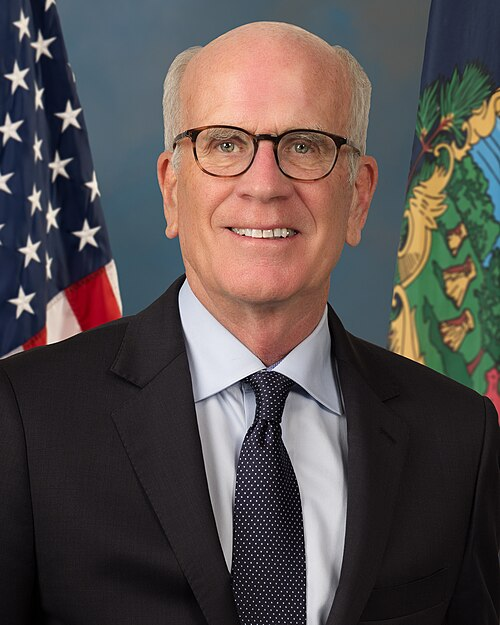
Co-Sponsor
Actions
2 actions
| Date | Action |
|---|---|
| Feb. 11, 2025 | Introduced in Senate |
| Feb. 11, 2025 | Read twice and referred to the Committee on Commerce, Science, and Transportation. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.