S. 2408: Access to Fertility Treatment and Care Act
The "Access to Fertility Treatment and Care Act" mandates that health insurance plans provide coverage for fertility treatments if they also offer coverage for obstetrical services. Here’s a breakdown of the key points of the bill:
Coverage Requirements
- Maintains that group health plans and health insurance issuers must cover fertility treatments, regardless of whether the individual has been diagnosed with infertility.
- Covers treatments including:
- Preservation of human oocytes, sperm, or embryos.
- Artificial insemination and various techniques like intravaginal insemination and intrauterine insemination.
- Assisted reproductive technologies such as in vitro fertilization.
- Genetic testing of embryos.
- Medications prescribed for fertility.
- Gamete donation.
- Other treatments and services deemed appropriate by the Secretary of Health and Human Services.
Cost Sharing and Limitations
- Any cost-sharing for fertility treatment cannot exceed the cost-sharing requirements applicable to other medical services.
- Prohibits plans from imposing stricter limitations on fertility treatment than on other medical services.
Prohibitions
- Plans cannot incentivize participants to avoid seeking treatments or penalize providers for offering such treatments.
- Providers must be allowed to discuss treatment options with patients.
- No discrimination against participants based on race, color, nationality, disability, or sex related to coverage.
Notification Requirements
- Health plans must inform participants about their fertility treatment coverage in written communications.
- Notifications should happen within specific deadlines following the effective date of the regulations.
Regulatory Framework
- The Secretary of Health and Human Services will develop appropriate regulations to implement these provisions.
- Other related health programs, such as Medicare and Medicaid, will align with these coverage requirements.
Impact on Specific Programs
- Federal Employees Health Benefits Program, TRICARE for military personnel, and Veterans Affairs health plans will also need to comply with these standards.
State Medicaid Plans
- This act requires state Medicaid plans to provide coverage for fertility treatment, ensuring compliance with the bill’s standards.
Effective Dates
- The provisions will generally take effect six months after the bill becomes law, with certain exceptions for collective bargaining agreements.
- Specific amendments regarding state Medicaid plans will take effect on October 1, 2026.
- Fertility treatment coverage under Medicare will begin for services provided on or after January 1, 2026.
Relevant Companies
- None found
This is an AI-generated summary of the bill text. There may be mistakes.
Show More
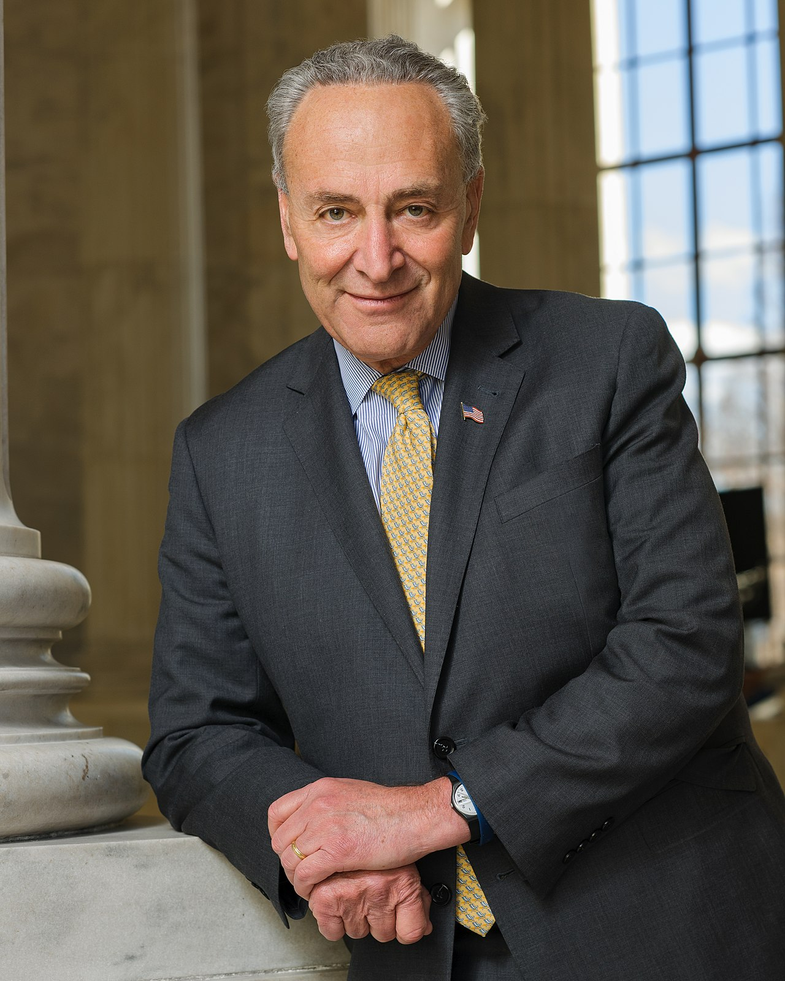
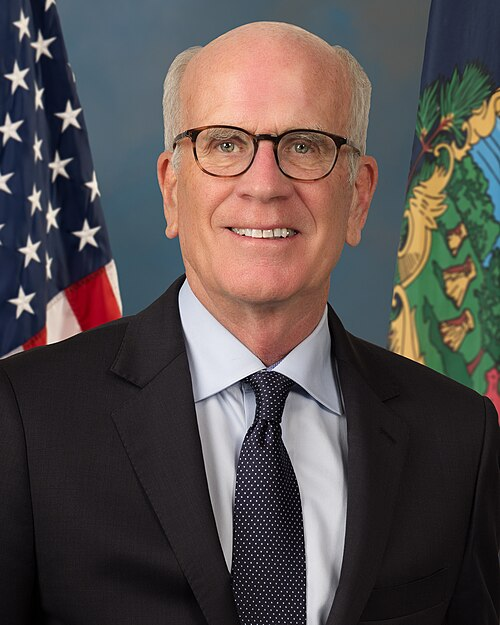
Sponsors
7 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Jul. 23, 2025 | Introduced in Senate |
| Jul. 23, 2025 | Read twice and referred to the Committee on Health, Education, Labor, and Pensions. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.
Potentially Relevant Congressional Stock Trades
No relevant congressional stock trades found.