H.R. 6423: Help Ensure Lower Patient Copays Act
The bill titled the "Help Ensure Lower Patient Copays Act" aims to modify health insurance regulations to allow for greater financial assistance in covering out-of-pocket costs for patients enrolled in group health plans or individual health insurance. Here’s a summary of the key provisions:
Financial Assistance Inclusion
The bill amends existing laws to specify that when establishing definitions of key terms related to health insurance costs, such as deductibles, coinsurance, copayments, and out-of-pocket limits, it will be required to include amounts that patients pay or amounts provided on their behalf. This includes:
- Financial assistance from non-profit organizations
- Assistance from prescription drug manufacturers
These amounts will be counted towards the individual’s deductible, coinsurance, copayment, or out-of-pocket limits.
Conforming Amendments
The bill also makes conforming changes to existing laws, which include:
- Amending the Patient Protection and Affordable Care Act (PPACA) to also recognize financial assistance in relation to deductibles and other expenses.
- Stipulating that limitations related to out-of-pocket expenditures for prescription drugs must reflect the inclusion of any financial assistance provided, thereby enhancing the benefits available to patients.
High Deductible Health Plans
Furthermore, the bill introduces provisions regarding high deductible health plans. It states that starting from plan years beginning after December 31, 2025, financial assistance will not prevent a health plan from being recognized as a high deductible health plan. This means that contributions towards out-of-pocket costs through assistance will count when determining if the necessary minimum deductible has been met.
Applicability
The amendments will pertain specifically to:
- Prescription drugs classified as specialty drugs
- Prescription drugs that are subject to utilization management
However, the use of tools such as prior authorization and step therapy will remain unaffected by these changes.
Effective Date
The changes proposed in this bill will take effect for group health plans and health insurance issuers for plan years beginning on or after January 1, 2026.
Relevant Companies
None found.
This is an AI-generated summary of the bill text. There may be mistakes.
Sponsors
27 bill sponsors
-
TrackThomas H. Kean, Jr.

Sponsor
-
TrackJake Auchincloss

Co-Sponsor
-
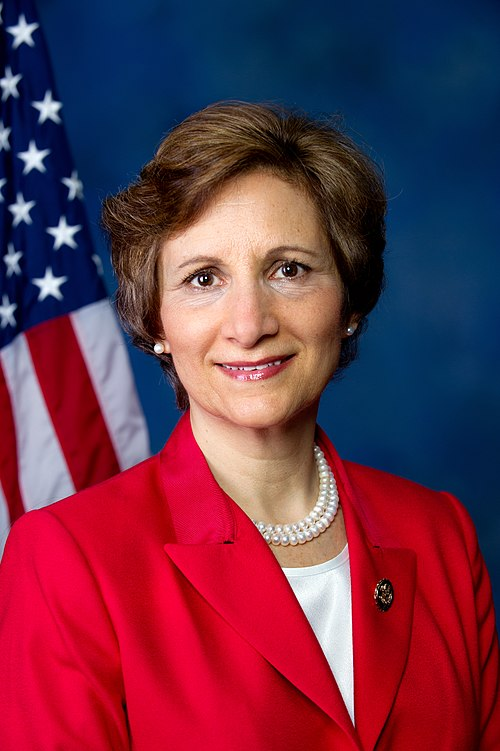
TrackNanette Diaz Barragán

Co-Sponsor
-
TrackSuzanne Bonamici
Co-Sponsor
-
TrackEd Case

Co-Sponsor
-
TrackJuan Ciscomani

Co-Sponsor
-
TrackSharice Davids

Co-Sponsor
-
TrackBrian K. Fitzpatrick

Co-Sponsor
-
TrackDaniel S. Goldman

Co-Sponsor
-
TrackJosh Gottheimer

Co-Sponsor
-
TrackMike Levin

Co-Sponsor
-
TrackTed Lieu
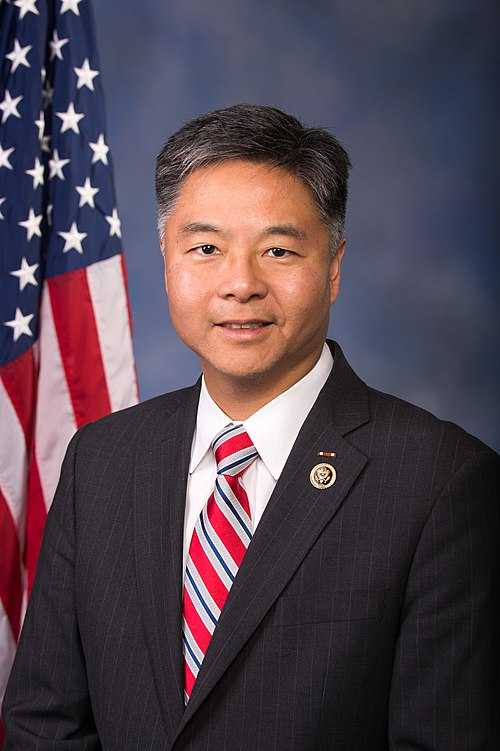
Co-Sponsor
-
TrackDoris O. Matsui

Co-Sponsor
-
TrackDaniel Meuser

Co-Sponsor
-
TrackMariannette Miller-Meeks
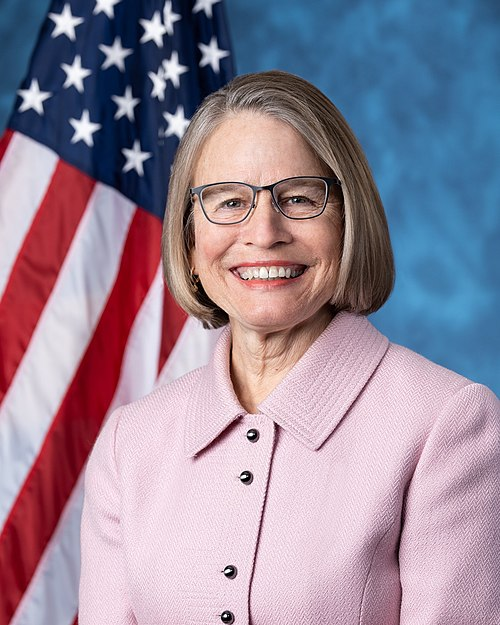
Co-Sponsor
-
TrackJimmy Panetta
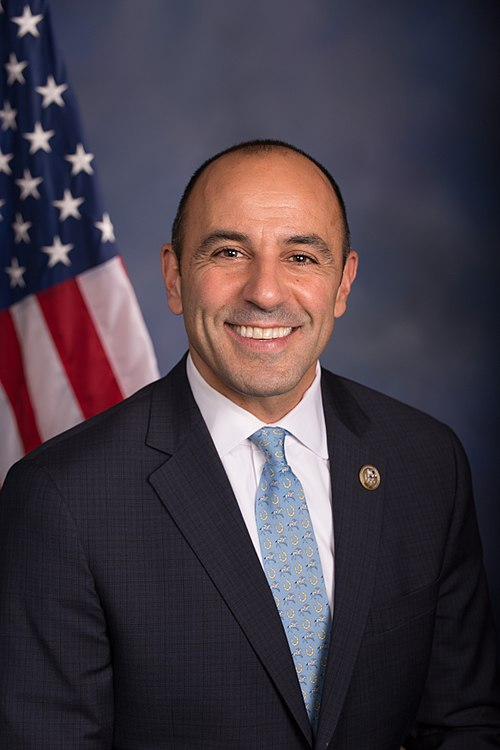
Co-Sponsor
-
TrackAugust Pfluger

Co-Sponsor
-
TrackMark Pocan
Co-Sponsor
-
TrackMike Quigley

Co-Sponsor
-
TrackDeborah K. Ross

Co-Sponsor
-
TrackMaria Elvira Salazar
Co-Sponsor
-
TrackLateefah Simon

Co-Sponsor
-
TrackHaley M. Stevens

Co-Sponsor
-
TrackSuhas Subramanyam

Co-Sponsor
-
TrackThomas R. Suozzi
Co-Sponsor
-
TrackBonnie Watson Coleman
Co-Sponsor
-
TrackJoe Wilson

Co-Sponsor
Actions
2 actions
| Date | Action |
|---|---|
| Dec. 04, 2025 | Introduced in House |
| Dec. 04, 2025 | Referred to the Committee on Energy and Commerce, and in addition to the Committee on Ways and Means, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.
Potentially Relevant Congressional Stock Trades
No relevant congressional stock trades found.