H.R. 5463: Choice Arrangement
This bill, titled the Choice Arrangement Act of 2025, proposes amendments to the Internal Revenue Code regarding employer-provided health reimbursement arrangements (HRAs) that are integrated with individual health insurance coverage. The key points of the bill include:
Integration of Health Reimbursement Arrangements
The bill allows health reimbursement arrangements to be considered compliant with various provisions of the Public Health Service Act if they meet specific criteria. These criteria include:
- The HRA must be funded solely by employer contributions and provide reimbursements for medical care during periods when the employee is covered under individual health insurance or Medicare.
- The HRA must adhere to nondiscrimination requirements, ensuring that all employees within a specified class (e.g., full-time, part-time) are offered the arrangement on the same terms.
- Employers can vary reimbursement amounts based on dependents covered or the age of the employee, with caps on total reimbursements related to age.
Substantiation and Notice Requirements
The bill establishes new substantiation requirements for HRAs. Employers must provide written notice to eligible employees about their rights and obligations regarding the arrangement at least 60 days before the plan year begins. This notice must be clear and comprehensible to the average employee.
Choice Arrangement Credit for Employers
The legislation introduces a tax credit for employers who establish a qualified CHOICE arrangement. The credit is calculated based on the number of months an employee is enrolled in the HRA, with specific amounts allocated for the first and second years of enrollment. Employers eligible for this credit are those who are not classified as "applicable large employers" under existing tax laws.
Tax Treatment and Reporting Requirements
The bill modifies existing tax code sections to include the total amount of benefits from qualified HRAs on employees' W-2 forms, ensuring that these amounts are clearly reported for tax purposes.
Effective Date
The amendments outlined in the bill are set to apply to plan years that begin after December 31, 2025.
Participants' Eligibility for Exchange Insurance
Additionally, the bill states that employees participating in these CHOICE arrangements may still be eligible to purchase insurance through the exchange without penalty, provided their employer offers a compliant arrangement.
Relevant Companies
- AET - Aetna, a major health insurance provider, could see changes in demand for its individual health insurance products as a result of this bill.
- UNH - UnitedHealth Group, a major player in health insurance and managed care, may also be influenced by the new HRA provisions and changes to employer health plans.
- ANTM - Anthem Inc., which offers various health insurance products, could be impacted by the integration of HRAs with individual insurance coverage.
This is an AI-generated summary of the bill text. There may be mistakes.
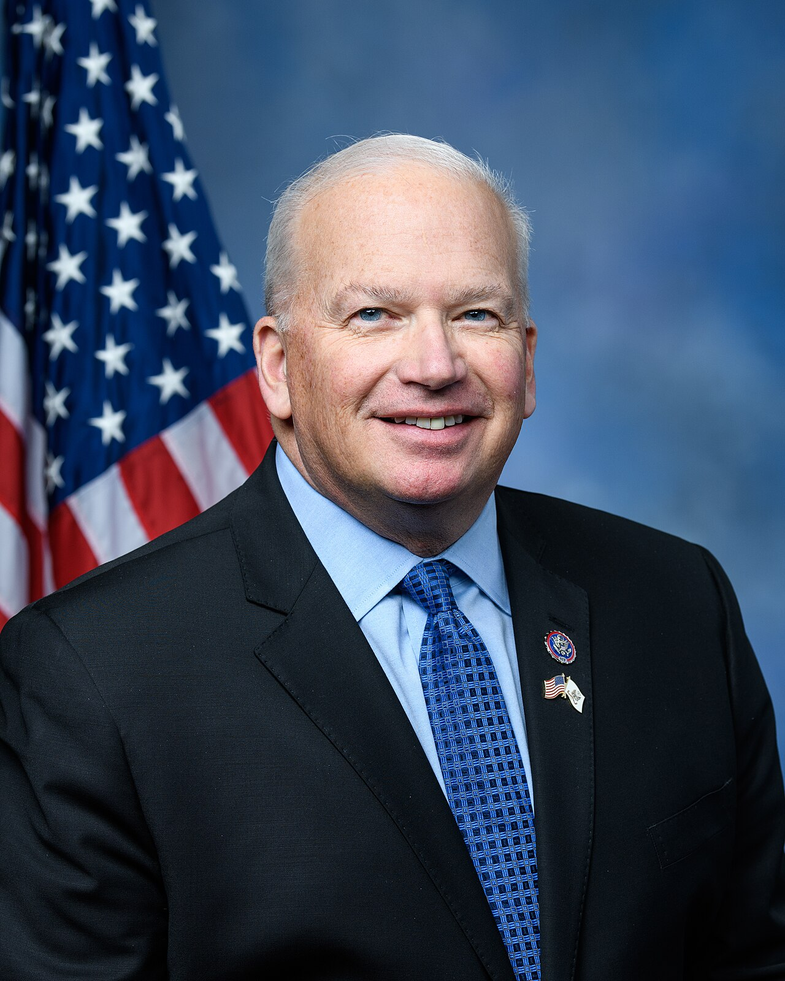
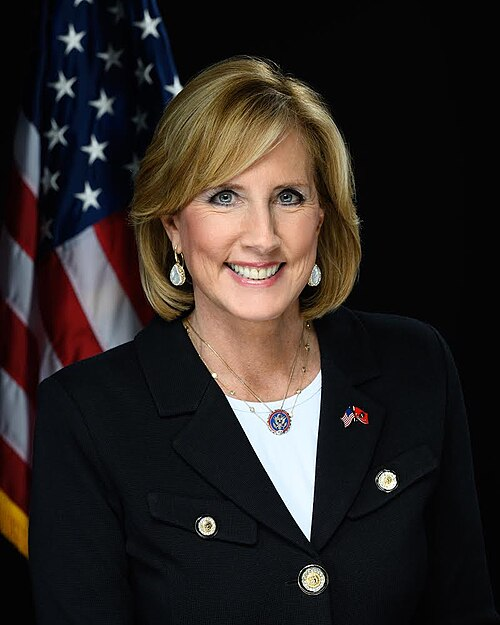
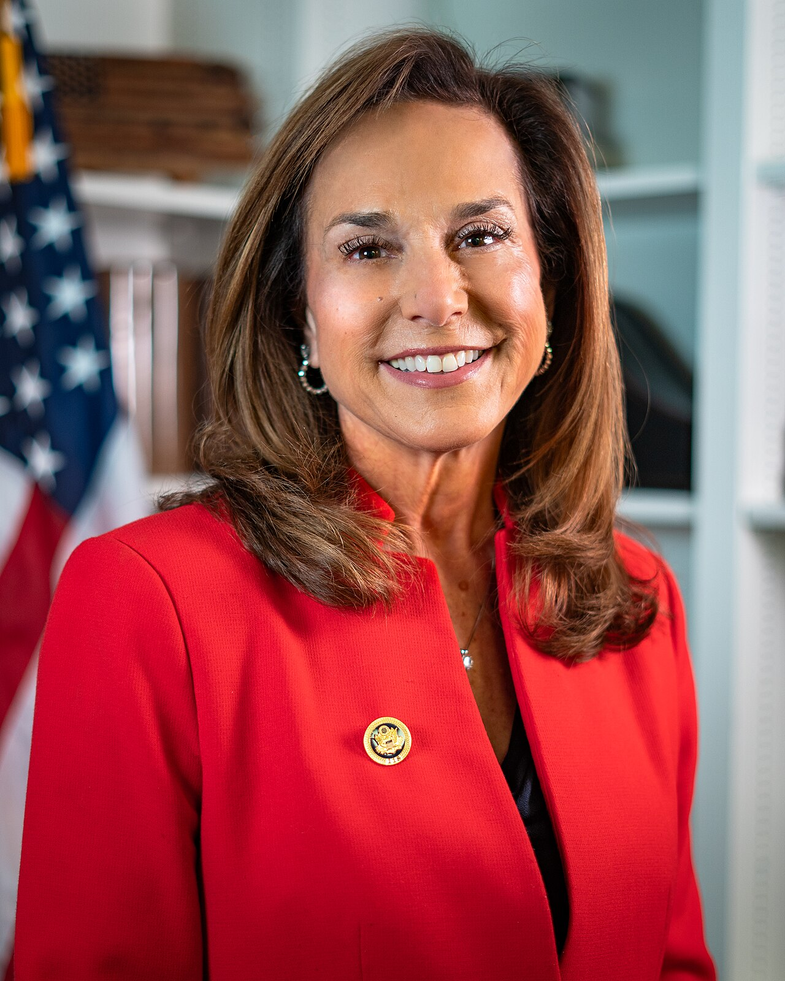
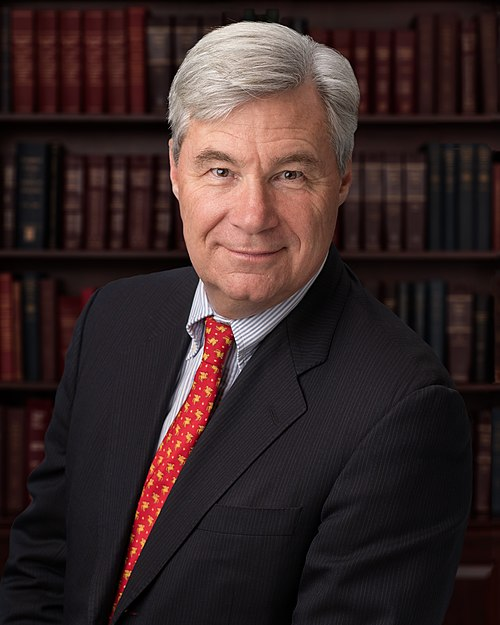
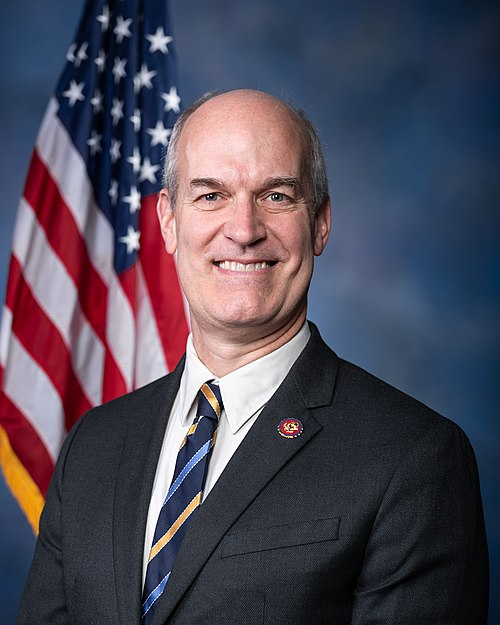
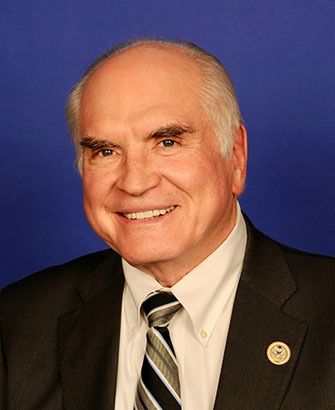
Sponsors
9 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Sep. 18, 2025 | Introduced in House |
| Sep. 18, 2025 | Referred to the House Committee on Ways and Means. |
Corporate Lobbying
2 companies lobbying