H.R. 4960: Beneficiary Enrollment Notification and Eligibility Simplification 2.0 Act
This bill, known as the Beneficiary Enrollment Notification and Eligibility Simplification 2.0 Act (or BENES 2.0 Act), aims to enhance the notification and enrollment processes for individuals approaching eligibility for Medicare. Below are the key provisions of the bill.
Eligibility and Enrollment Notifications
The bill mandates that the Social Security Administration (SSA) provides information to individuals aged 60 to 65 regarding their eligibility for Medicare benefits. Specifically, changes include:
- Inclusion of Medicare Information: When Social Security account statements are sent to individuals nearing Medicare eligibility, these statements must include details about Medicare benefits, including:
- Eligibility criteria for benefits under Medicare Part B.
- Information about late enrollment penalties, including how they are calculated and potential relief options.
- Coordination of benefits for individuals with special considerations (e.g., veterans, low-income individuals).
- Contact information for further assistance, such as the Medicare helpline and SSA resources.
- Notice Development: The bill requires the Secretary of Health and Human Services to develop this notice within a year after collecting input from stakeholders, including seniors, veterans, and health insurers. The notice will be reviewed and potentially modified every two years to ensure its relevance and effectiveness.
- Posting Requirements: The SSA and Medicare must post this information on their official websites to ensure easy public access.
Timing of Statements
The bill stipulates that the Social Security account statements for individuals turning 65 should be mailed at least three months but not more than six months before their birthday. This timing is intended to ensure that individuals have adequate notice to enroll in Medicare before they reach eligibility age.
Notices for Social Security Beneficiaries
The bill also extends the requirements for notice distribution to those currently receiving Social Security benefits. It ensures that these beneficiaries receive the same information regarding Medicare eligibility before they become eligible for Medicare.
Authority to Modify Notices
The Secretary of Health and Human Services has the authority to modify the notice content based on feedback from the target population. This approach allows for updates and improvements over time to better meet the needs of individuals approaching Medicare eligibility.
Relevant Companies
- None found
This is an AI-generated summary of the bill text. There may be mistakes.
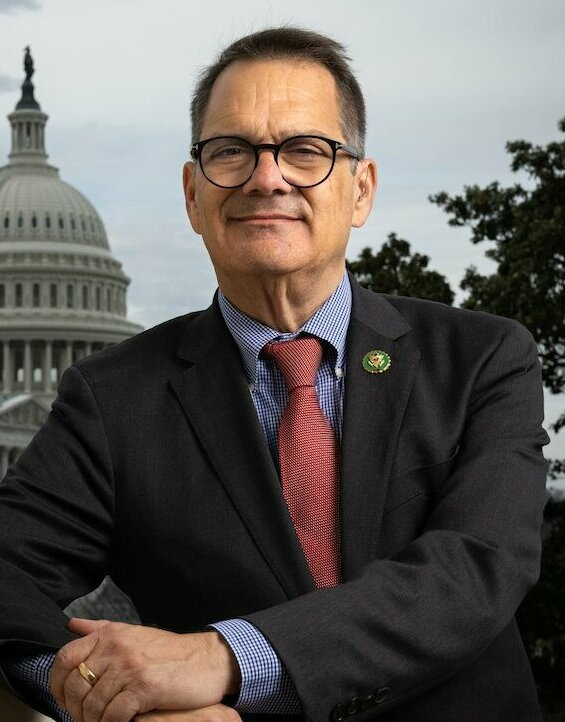
Sponsors
4 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Aug. 12, 2025 | Introduced in House |
| Aug. 12, 2025 | Referred to the Committee on Ways and Means, and in addition to the Committee on Energy and Commerce, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.
Potentially Relevant Congressional Stock Trades
No relevant congressional stock trades found.