H.R. 4745: Medicaid Bump Act
This bill, known as the Medicaid Bump Act, aims to amend the Social Security Act to increase federal funding for behavioral health services provided through Medicaid. Here are the main components of the bill:
Higher Federal Matching Rate
The bill proposes to raise the federal matching rate for states that increase their Medicaid spending on behavioral health services, which includes mental health care and substance use treatment. Specifically, if a state’s current spending exceeds certain benchmarks based on expenditures from a previous period (the four-quarter period ending March 31, 2019), the federal government would match 90% of that increase.
Accountability and Maintenance of Effort
To ensure that states do not reduce their own funding in lieu of federal funding, the bill includes conditions for receiving this additional federal funding:
- Supplement, not supplant: States must use these federal funds to supplement, not replace, the state funds allocated for behavioral health services that were in place as of April 1, 2021.
- Use of funds for improvement: States are required to utilize the funds for activities that enhance the availability and quality of behavioral health services, which may include raising payment rates for providers and implementing measures to reduce staff turnover.
Guidance from Health and Human Services
The bill mandates that the Secretary of Health and Human Services must issue guidance to the states within 180 days after the bill becomes law. This guidance will clarify which services are categorized as behavioral health services under the new regulations.
Effective Date
The amendments proposed in this bill would take effect for calendar quarters starting January 1 of the year following the bill's enactment.
Annual Reporting Requirements
Additionally, the Secretary of Health and Human Services is required to submit an annual report to both the House Committee on Energy and Commerce and the Senate Committee on Finance. This report will include details on behavioral health services provided under Medicaid, covering payment rates, the rationale behind those rates, and the utilization of such services in each state.
Relevant Companies
- None found
This is an AI-generated summary of the bill text. There may be mistakes.
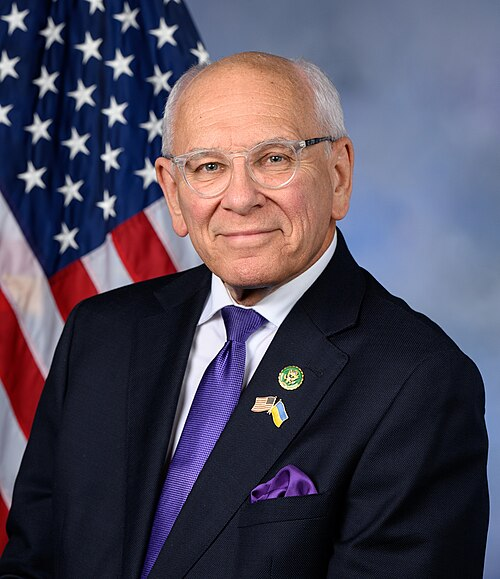
Sponsors
3 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Jul. 23, 2025 | Introduced in House |
| Jul. 23, 2025 | Referred to the House Committee on Energy and Commerce. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.
Potentially Relevant Congressional Stock Trades
No relevant congressional stock trades found.