H.R. 4406: State-Based Universal Health Care Act of 2025
This bill, known as the State-Based Universal Health Care Act of 2025, aims to create a framework that allows individual states to develop and implement their own comprehensive universal health care systems. The key points of the bill include:
Objective
The main goal of this legislation is to provide states with the flexibility to establish their own health care systems that offer comprehensive health benefits to all residents.
State Waivers
States can apply for a waiver from certain federal requirements related to health benefits coverage. This waiver would enable states to design their own health care plans that meet specific criteria, with full implementation beginning on January 1, 2026.
Application Process
The application for a waiver must include:
- A description of the state legislation or legal authority for the proposed health care plan.
- A plan to cover at least 95% of residents within five years.
- A budget that ensures the plan is neutral for federal spending.
Funding and Resource Management
Under the waiver, federal funds that would have been allocated to traditional federal health programs would instead be redirected to the states to support their health care systems. States will also have access to any administrative savings from health care spending to reinvest in their health care services.
Requirements for Approval
The Secretary of Health and Human Services will grant waivers if the proposed plans:
- Provide health benefits coverage that is as comprehensive as existing federal programs.
- Offer protections against excessive out-of-pocket costs.
- Ensure coverage for all residents, including those traditionally covered by federal programs.
- Are publicly administered by state agencies or independent public entities.
Monitoring and Review
States receiving waivers must submit reports every five years to assess the effectiveness of their health care systems, including metrics such as coverage rates, affordability, and overall health improvements. Failure to achieve the goal of 95% coverage may result in technical assistance from the federal government or potential termination of the waiver.
Independent Assessment Panel
The bill establishes an Independent Assessment Panel to review waiver applications and provide recommendations. This panel will consist of representatives from various health and governance sectors and will report on the status of waivers annually to Congress.
Special Provisions for Indian Health Care
Specific guidance will be provided regarding the application of this act to ensure that health services to American Indians and Alaska Natives are maintained without enrollment fees or similar charges. States must also contract with Indian health care providers effectively.
Definitions and Scope
The bill outlines definitions for terms like "health benefits coverage," "resident," and "Secretary," and specifies federally recognized health programs involved.
Conclusion Clause
Overall, the bill enables states to pursue more tailored health care solutions, transitioning away from federal mandates while ensuring comprehensive protections and access for residents.
Relevant Companies
None found.
This is an AI-generated summary of the bill text. There may be mistakes.
Sponsors
30 bill sponsors
-
TrackRo Khanna

Sponsor
-
TrackYassamin Ansari

Co-Sponsor
-
TrackSuzanne Bonamici
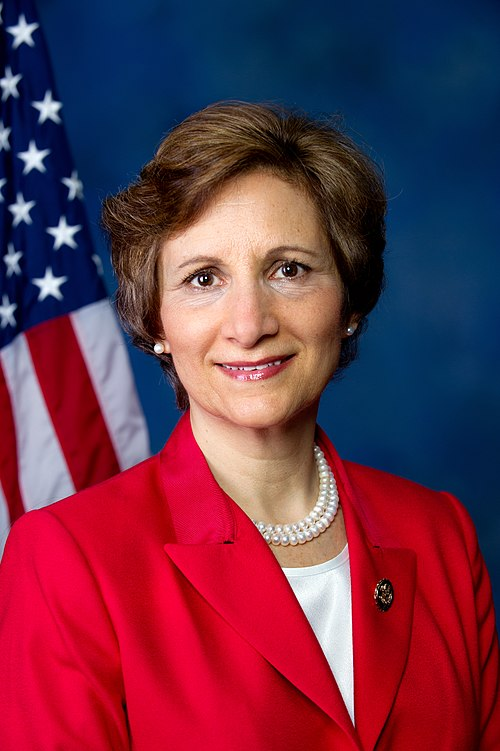
Co-Sponsor
-
TrackSheila Cherfilus-McCormick

Co-Sponsor
-
TrackYvette D. Clarke
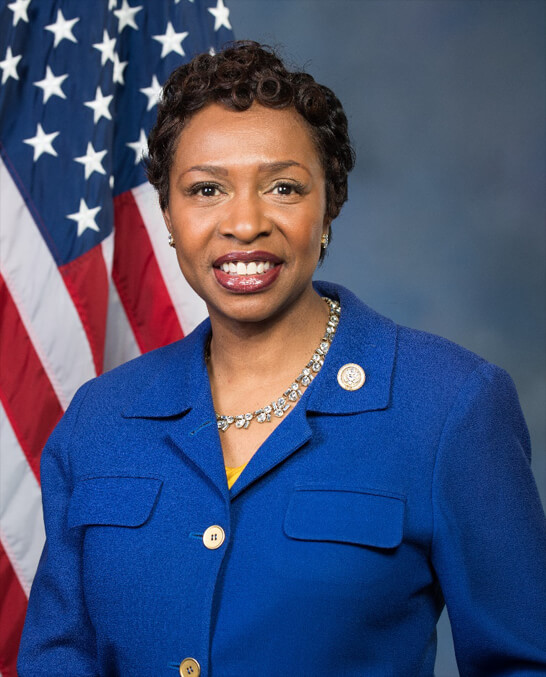
Co-Sponsor
-
TrackSteve Cohen

Co-Sponsor
-
TrackMaxine Dexter

Co-Sponsor
-
TrackMaxwell Frost

Co-Sponsor
-
TrackVal T. Hoyle

Co-Sponsor
-
TrackJared Huffman
Co-Sponsor
-
TrackPramila Jayapal

Co-Sponsor
-
TrackSummer L. Lee

Co-Sponsor
-
TrackJames P. McGovern

Co-Sponsor
-
TrackJerrold Nadler
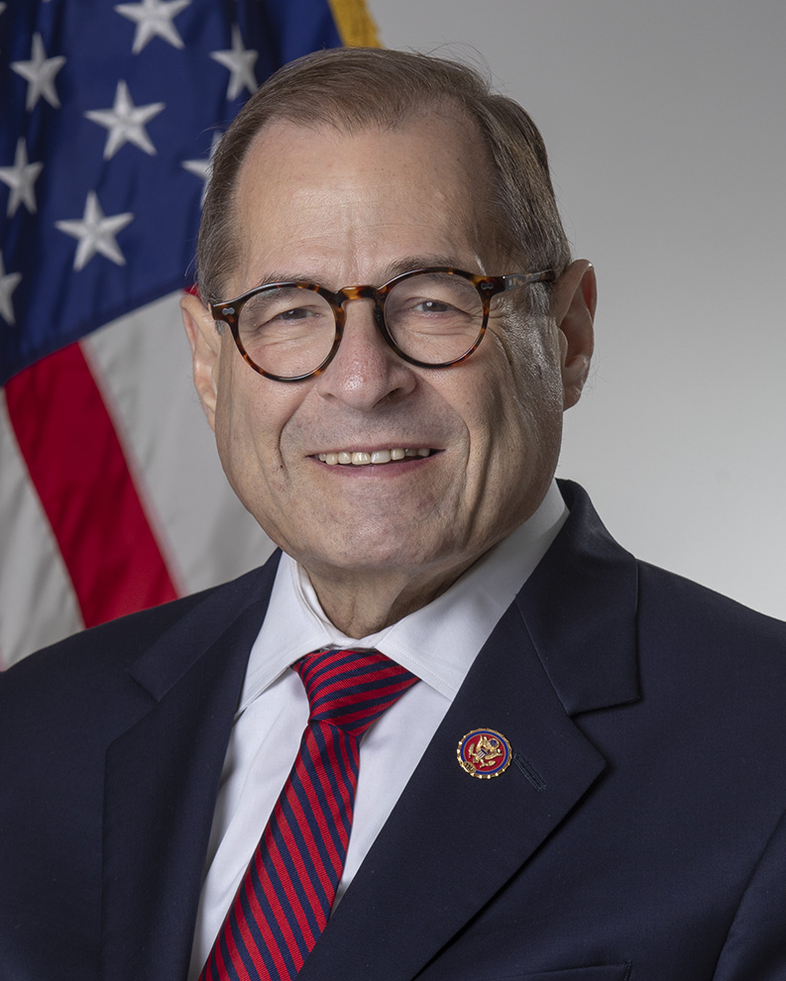
Co-Sponsor
-
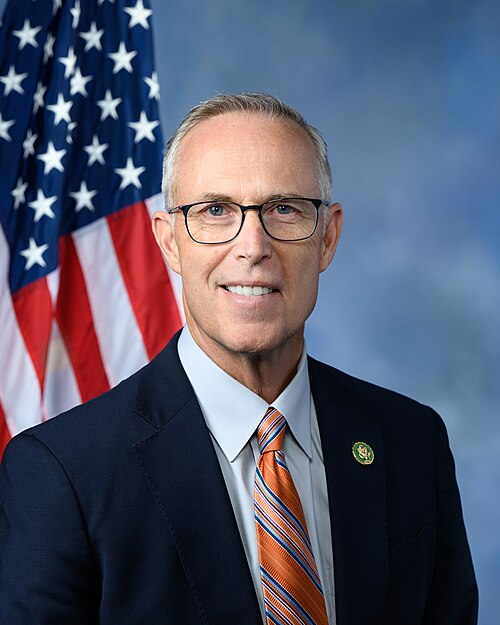
TrackJoe Neguse

Co-Sponsor
-
TrackEleanor Holmes Norton

Co-Sponsor
-
TrackIlhan Omar

Co-Sponsor
-
TrackChellie Pingree

Co-Sponsor
-
TrackMark Pocan
Co-Sponsor
-
TrackAyanna Pressley

Co-Sponsor
-
TrackDelia C. Ramirez

Co-Sponsor
-
TrackAndrea Salinas
Co-Sponsor
-
TrackJanice D. Schakowsky
Co-Sponsor
-
TrackAdam Smith
Co-Sponsor
-
TrackMelanie A. Stansbury

Co-Sponsor
-
TrackShri Thanedar

Co-Sponsor
-
TrackBennie G. Thompson
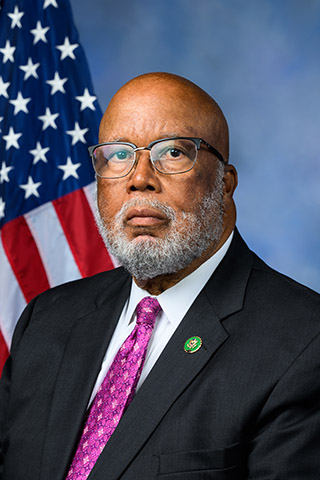
Co-Sponsor
-
TrackRashida Tlaib

Co-Sponsor
-
TrackNydia M. Velázquez

Co-Sponsor
-
TrackBonnie Watson Coleman
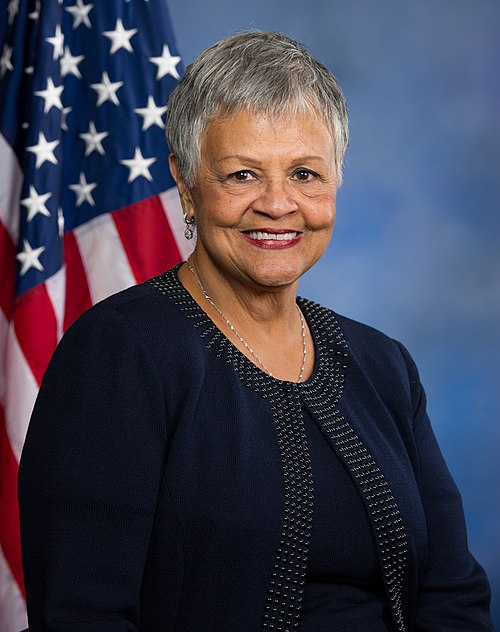
Co-Sponsor
Actions
2 actions
| Date | Action |
|---|---|
| Jul. 15, 2025 | Introduced in House |
| Jul. 15, 2025 | Referred to the Committee on Energy and Commerce, and in addition to the Committees on Armed Services, Ways and Means, Oversight and Government Reform, and Education and Workforce, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.
Potentially Relevant Congressional Stock Trades
No relevant congressional stock trades found.