H.R. 4056: Repair Abuses of MSP Payments Act
This bill, titled the Repair Abuses of MSP Payments Act (RAMP Act), aims to amend the Social Security Act, specifically concerning how group health plans handle payments related to Medicare. Here’s what the bill seeks to achieve:
Changes to Payment Responsibilities
The bill modifies the existing framework that governs how group health plans are required to pay for medical services when Medicare is also involved. It specifically shifts the terminology from "primary plan" to "group health plan." This means that if a group health plan fails to make appropriate payments for services when it is supposed to act as the primary payer, individuals will have the right to pursue legal action for damages.
Intent of the Legislation
The intention behind this bill is to improve accountability among group health plans regarding their payment responsibilities. By allowing legal recourse, the authors of the bill aim to ensure that individuals seeking coverage do not face financial hardships due to delays or failures in payment by their health plans, thus protecting beneficiaries’ rights.
Legal Action Provisions
With this legislation, affected individuals could potentially sue group health plans if they can demonstrate that their plan failed to provide necessary reimbursements or primary payments. This serves as a mechanism to address grievances for situations where people may be left with unpaid medical bills due to the inaction of their health plan.
Impact Scope
This bill pertains specifically to group health plans, which are typically employer-sponsored insurance plans. This means that the primary focus is on health insurance provided by employers rather than individual plans. The changes would be enforced under Medicare’s coordination of benefits rules.
Relevant Companies
- UNH - UnitedHealth Group: As a large health insurance provider, any changes in legal liability related to payment responsibilities could significantly impact their operational procedures and potential liabilities.
- ANTM - Anthem, Inc.: Similar to UnitedHealth, Anthem could see legal consequences and operational adjustments based on the implementation of risks associated with delayed payments or administrative errors.
- HUM - Humana Inc.: Humana might be affected by increased claims against them for reimbursement issues if the bill leads to more lawsuits from members regarding payment failures.
This is an AI-generated summary of the bill text. There may be mistakes.
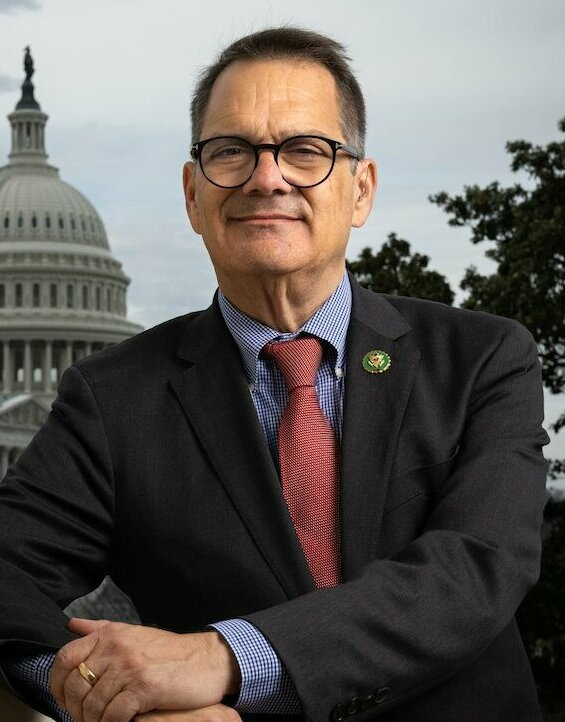
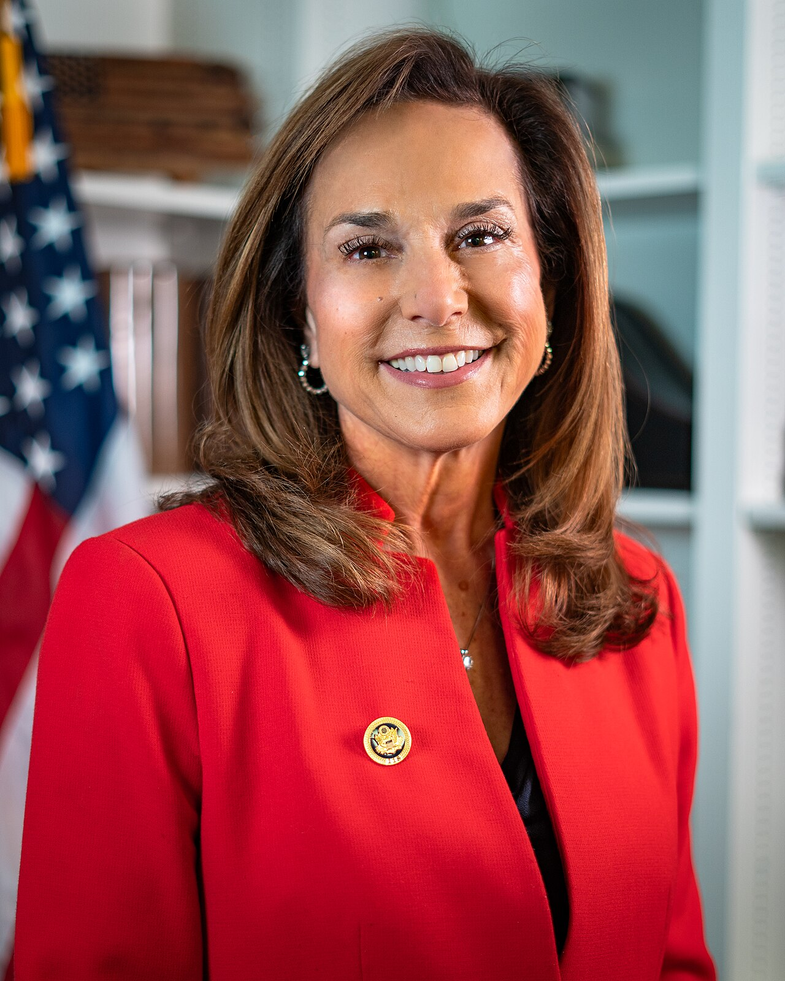
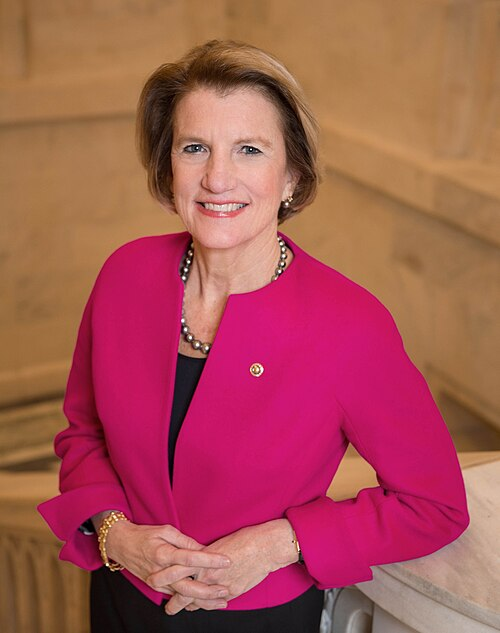
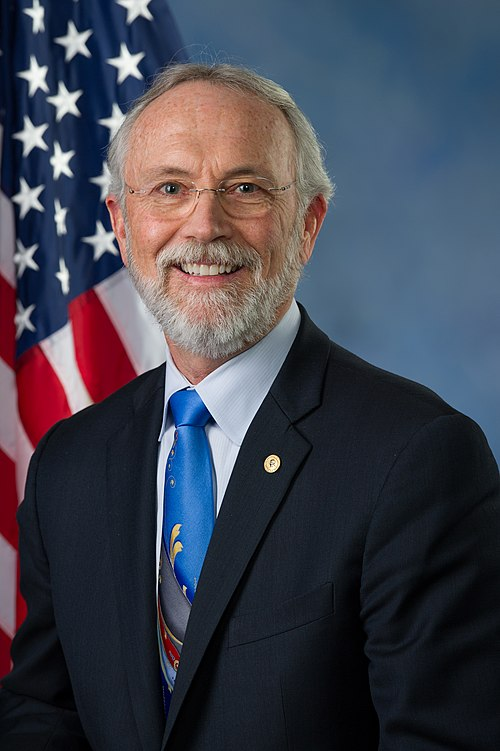
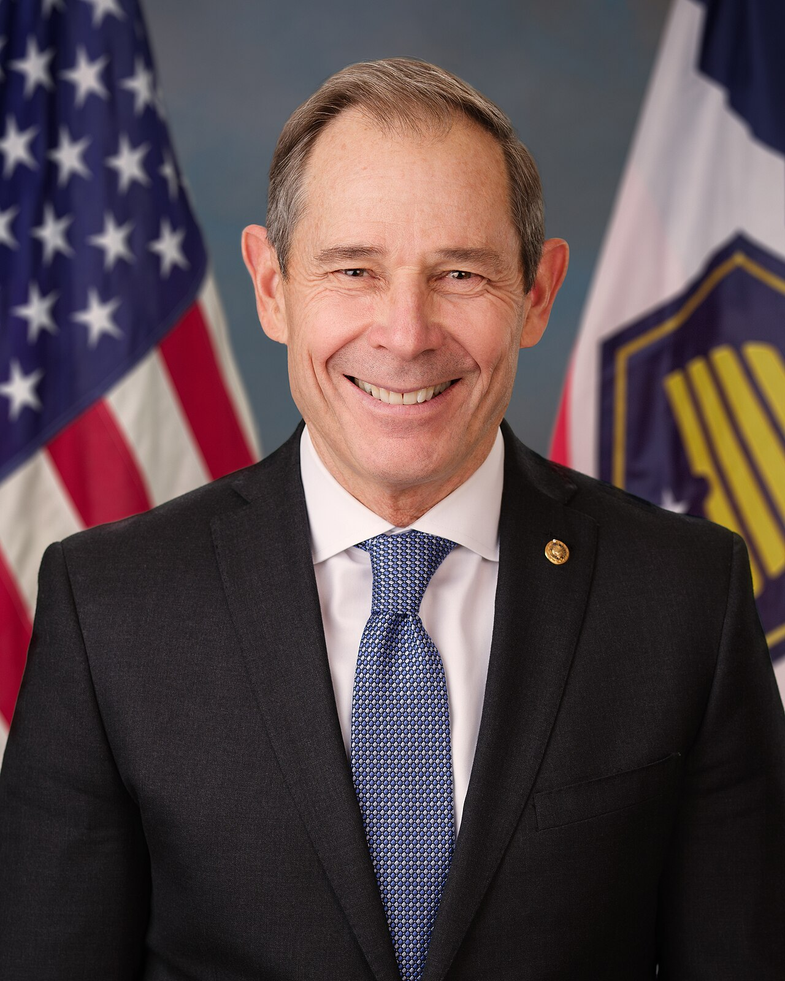
Sponsors
2 bill sponsors
Actions
2 actions
| Date | Action |
|---|---|
| Jun. 20, 2025 | Introduced in House |
| Jun. 20, 2025 | Referred to the Committee on Ways and Means, and in addition to the Committee on Energy and Commerce, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
1 company lobbying