H.R. 3037: Access to Breast Cancer Diagnosis Act of 2025
This bill, titled the Access to Breast Cancer Diagnosis Act of 2025, aims to enhance accessibility to breast cancer diagnostic and supplemental examinations for individuals with group or individual health insurance coverage. Here’s a summary of its main points:
Key Provisions
- Cost-Sharing Requirements Prohibition: The bill mandates that group health plans and health insurance issuers cannot impose any cost-sharing requirements on benefits related to diagnostic and supplemental breast examinations. This means that individuals receiving these services will not need to pay deductibles, copayments, or coinsurance for such exams.
- Types of Examinations Covered:
- Diagnostic Breast Examinations: These are necessary examinations following an abnormality found in a screening, utilizing methods like mammography or MRI.
- Supplemental Breast Examinations: These are screenings for breast cancer that occur without a prior indication of abnormality but are based on personal or family risk factors.
- Utilization Controls: The bill allows health plans to require prior authorization or implement other utilization controls for coverage of these examinations, ensuring that services are used appropriately.
- State Law Considerations: The bill clarifies that it does not override state laws that may provide better coverage protections or requirements for diagnostic and supplemental breast examinations.
- Grandfathered Health Plans: The bill modifies existing provisions to ensure that grandfathered plans under the Affordable Care Act also adhere to these new coverage mandates for breast examinations.
- High Deductible Health Plans (HDHPs): It provides a safe harbor to HDHPs by stating that having no deductible for these breast examinations does not affect a plan's status as a high deductible health plan, starting from plan years beginning on or after January 1, 2026.
Effective Date
The provisions outlined in this bill will take effect for plan years starting on or after January 1, 2026.
Definitions
The bill defines several key terms to ensure clarity, such as:
- Cost-sharing requirements: This includes any out-of-pocket expenses that a patient might incur, such as deductibles and coinsurance.
- Diagnostic breast examination: A breast examination deemed necessary when there is a suspicion or detection of an abnormality through other examinations.
- Supplemental breast examination: A breast examination aimed at screening for cancer based on risk factors without prior suspicion of abnormalities.
Relevant Companies
- RMD: As a company involved in radiology and imaging technologies, RMD may see increased demand for their breast imaging products and services due to expanded testing resulted from this bill.
- GE: General Electric, known for its medical devices and imaging technologies, could be impacted by increased utilization of MRI and ultrasound machines for breast examinations.
This is an AI-generated summary of the bill text. There may be mistakes.
Sponsors
21 bill sponsors
-
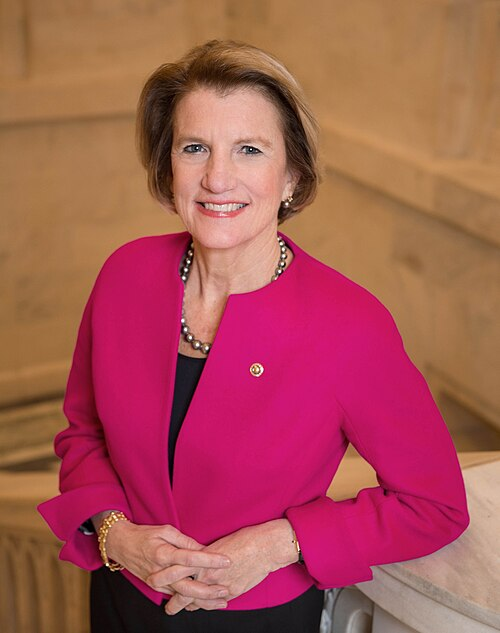
TrackDebbie Dingell

Sponsor
-
TrackRobert Bresnahan

Co-Sponsor
-
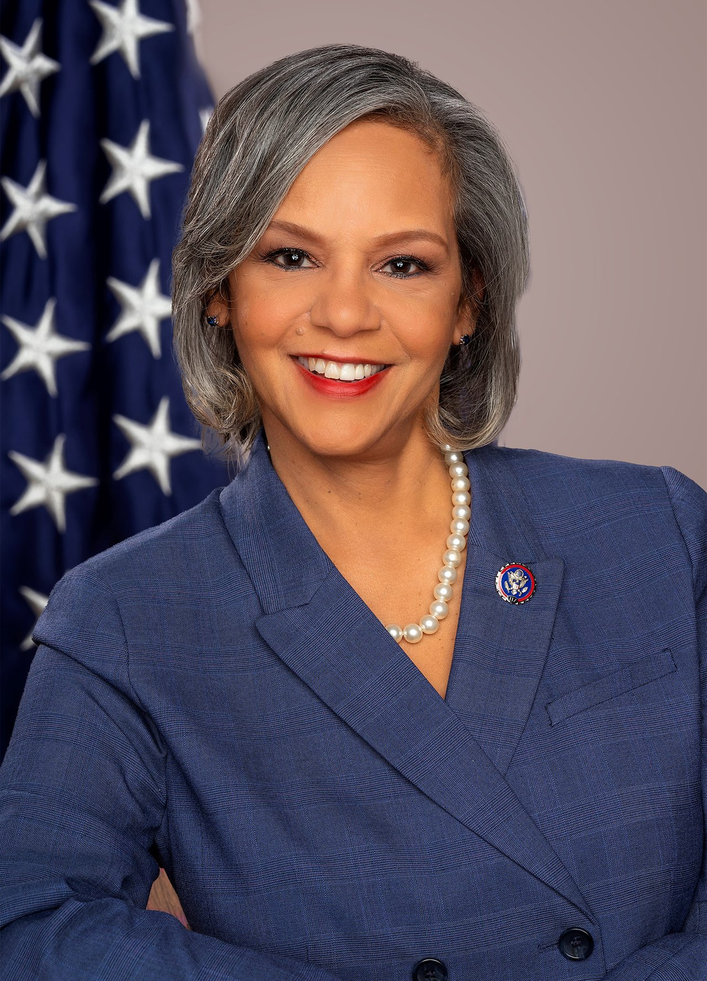
TrackYvette D. Clarke
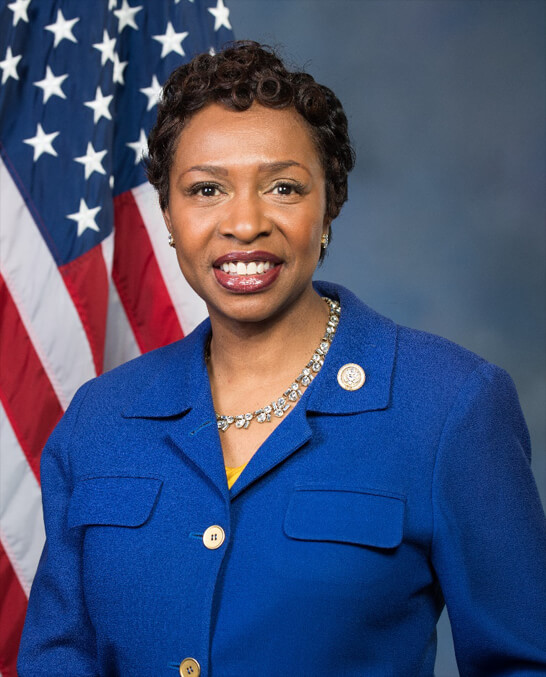
Co-Sponsor
-
TrackAngie Craig
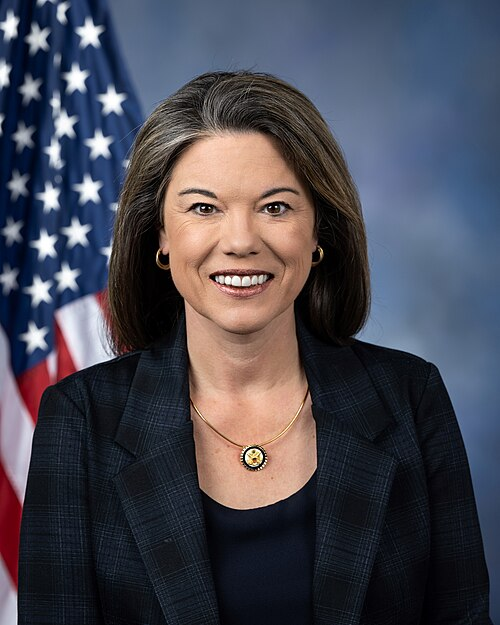
Co-Sponsor
-
TrackLloyd Doggett
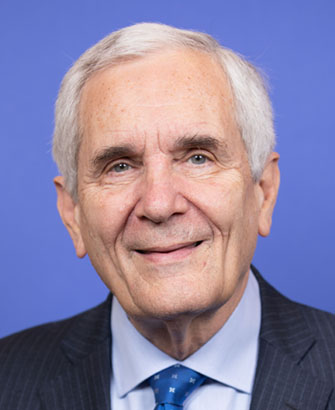
Co-Sponsor
-
TrackBrian K. Fitzpatrick

Co-Sponsor
-
TrackJahana Hayes

Co-Sponsor
-
TrackThomas H. Kean, Jr.

Co-Sponsor
-
TrackRobin L. Kelly
Co-Sponsor
-
TrackTimothy M. Kennedy

Co-Sponsor
-
TrackGreg Landsman

Co-Sponsor
-
TrackJohn B. Larson

Co-Sponsor
-
TrackMichael Lawler

Co-Sponsor
-
TrackJennifer L. McClellan

Co-Sponsor
-
TrackGwen Moore

Co-Sponsor
-
TrackSeth Moulton

Co-Sponsor
-
TrackEleanor Holmes Norton

Co-Sponsor
-
TrackScott H. Peters

Co-Sponsor
-
TrackMelanie A. Stansbury

Co-Sponsor
-
TrackPaul Tonko
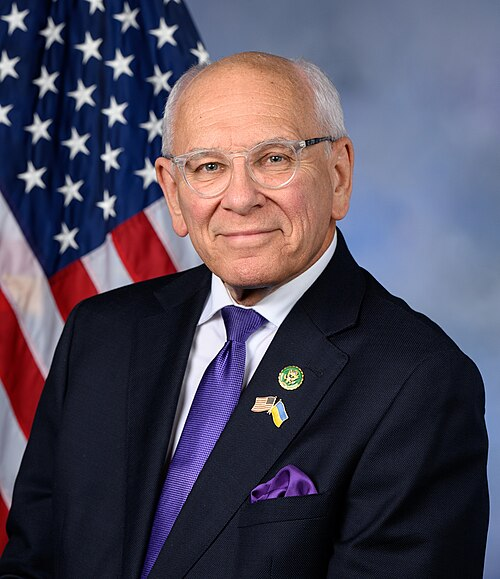
Co-Sponsor
-
TrackDebbie Wasserman Schultz
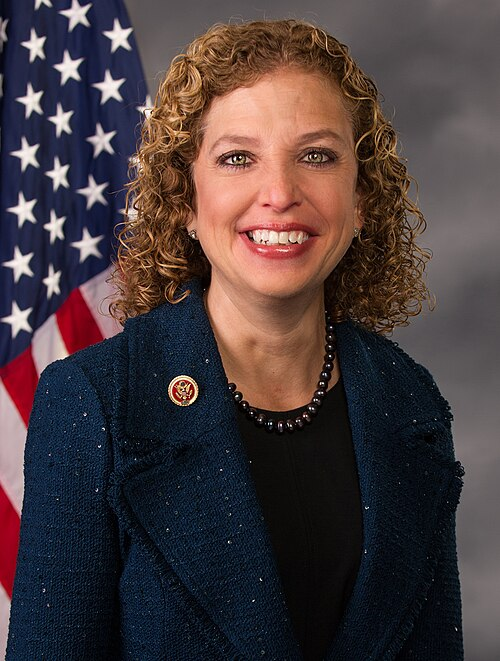
Co-Sponsor
Actions
2 actions
| Date | Action |
|---|---|
| Apr. 28, 2025 | Introduced in House |
| Apr. 28, 2025 | Referred to the Committee on Energy and Commerce, and in addition to the Committee on Ways and Means, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned. |
Corporate Lobbying
0 companies lobbying
None found.
* Note that there can be significant delays in lobbying disclosures, and our data may be incomplete.